 |
| No causal effect of RA on glaucoma was found in the East Asian population, but there was a positive association between RA and glaucoma in the European population. Photo: iStock. Click image to enlarge. |
Though seemingly unrelated, numerous studies have pointed to potential causal associations that exist between cataract, glaucoma and rheumatoid arthritis (RA). However, it remains unclear whether RA is indeed a directly influencing underlying condition that raises risks for cataract or glaucoma. In a new genetic analysis, study researchers investigated the relationship of these conditions in European and East Asian populations.
Genome-wide association study (GWAS) summary statistics were collected for cataract from 372,386 individuals and glaucoma from 377,277 individuals in the European population. RA summary data in this population was derived from a meta-analysis of GWAS comprising 97,173 samples. The East Asian study population comprised 212,453 individuals for cataract and glaucoma and 22,515 individuals for RA.
Identified were between eight and 56 single-nucleotide polymorphisms suited for investigation, depending on the condition. After analysis, the study researchers revealed that RA had an increased risk of cataract and glaucoma in the European population. RA only showed a positive association with cataract in the East Asian population. The authors “believe that oxidative stress and local inflammation are responsible for these causal associations,” and they expand upon this statement in their discussion. However, it should be noted that reverse MR analyses suggested that cataract and glaucoma had no causal effect on RA.
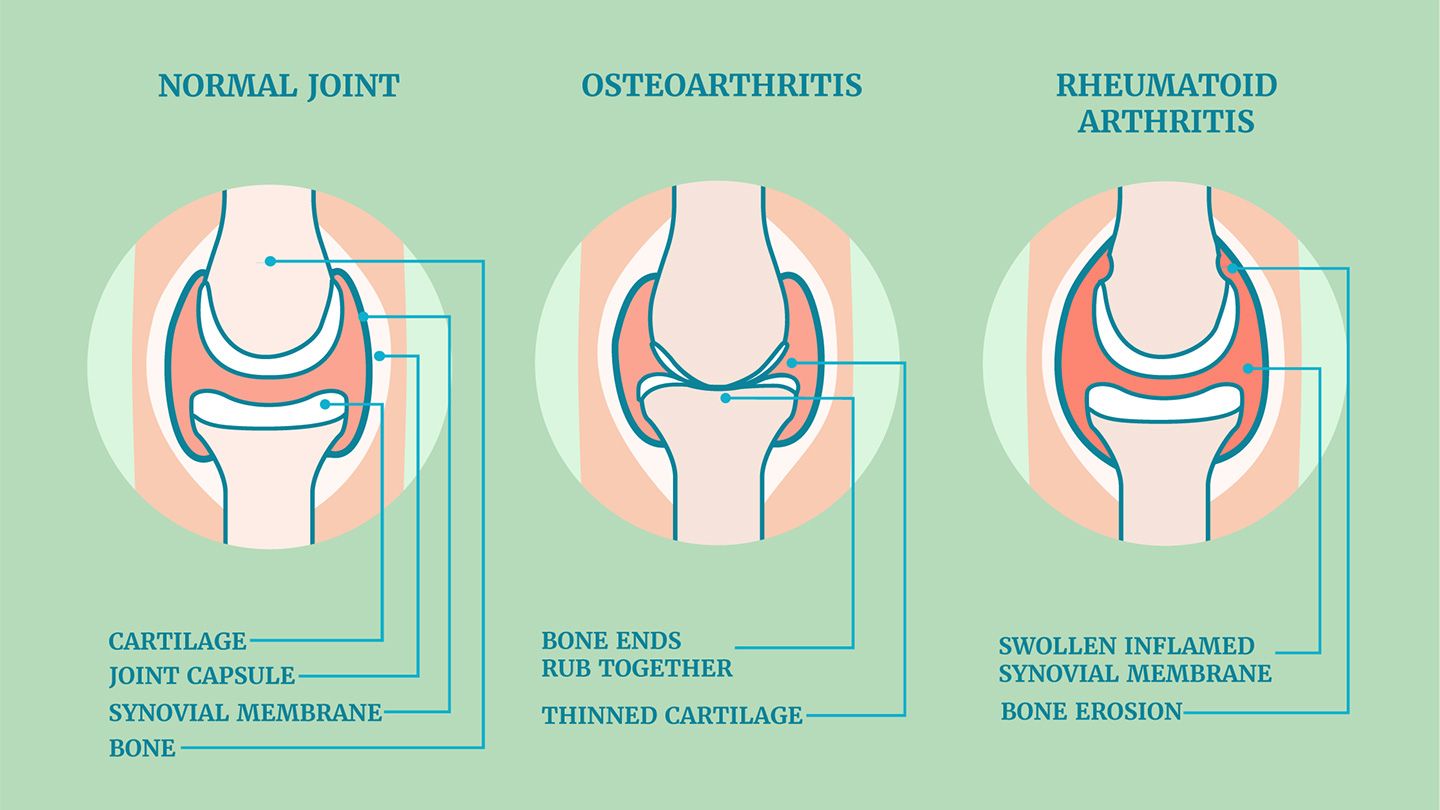
Characterized by inflammatory changes in the synovial membrane of joints and erosive arthritis, RA has more recently gained increasing attention due to oxidative stress, which is thought to be a key player in development of the condition. Both the mitochondria and blood of RA patients have exhibited elevated levels of reactive oxygen species, which is a prominent biomarker of oxidative stress. Subsequently, these species can cause damage to articular cartilage either directly or indirectly, leading to proteoglycan degradation and inhibition of their synthesis. Pathogenesis of cataract is also related to oxidative stress, with an imbalance in the lens’ redox state driven by this stress and contributing to development. As well, oxidative stress accelerates lens epithelial cell loss, also a critical factor in cataract development.
Shifting to other aspects of the disease, RA also involves local inflammation as a central element in its development. Inflammatory factors and chemokines of tumor necrosis factor, interleukins and matrix metalloproteinase are all upregulated in synovial macrophages and dendritic cell subsets in RA patients. With this upregulation, the inflammatory mediators lead to cartilage degradation, bone erosion and accelerated RA development. Inflammation also plays a critical role in glaucoma pathogenesis. The same inflammatory factors of tumor necrosis factor, two different interleukins and matrix metalloproteinase can all promote retinal ganglion cell death—a hallmark of glaucoma development.
The authors are hopeful that their results may “offer guidance in the early prevention of cataract and glaucoma in RA patients and provide some evidence for the RA-induced inflammation on ophthalmic diseases.”
Teng M, Wang J, Su X, et al. Causal associations between rheumatoid arthritis, cataract and glaucoma in European and East Asian populations: a bidirectional two-sample mendelian randomization study. PLoS ONE. 2024;19(3):e0299192. |


