 |
|
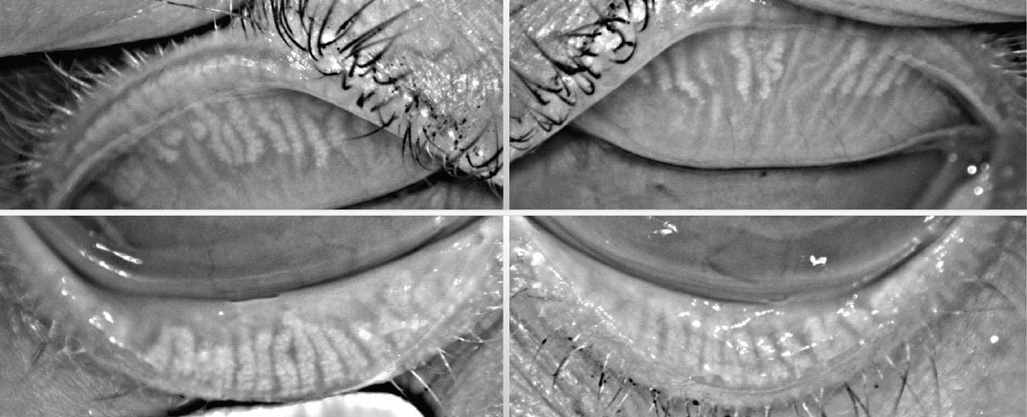
Higher prevalence and increased severity of MGD was found in patients with both type 2 diabetes and DED compared with those only with DED. Photo: Katherine Sanford, OD. Click image to enlarge. |
While studies have been conducted on the effects of diabetes on tear film and secretion, few have focused on the impact of diabetes on meibomian gland (MG) morphology and function. In this study, researchers evaluated the impact of type 2 diabetes mellitus (T2DM) on dry eye disease (DED) and found that higher prevalence and increased severity of MG dysfunction (MGD) was found in patients with both T2DM and DED compared with those only with DED.
A total of 90 individuals were divided into four groups: DM patients with DED (n = 30), DM patients without DED (n = 18), DED patients without DM (n = 26) and controls (n = 16). All were administered the ocular surface disease index (OSDI) questionnaire, tear meniscus height, noninvasive Keratograph tear film breakup time, Schirmer I test, corneal fluorescein staining, eyelid margin abnormality examinations, meibum quality and MG dropout evaluations.
“We observed that the MG loss was significantly higher in both the upper and lower eyelids of diabetics with DED than in nondiabetics with DED,” the study authors wrote in their paper. “The score of either lid margin abnormality or meibum quality was not correspondingly significantly higher, but these two variables are just an indirect reflection of MGD.”
A previous study observed that the nonobvious MGD subtype with severe MG loss had normal lipid secretion, with the authors speculating that few but active MGs could maintain meibum expression. This might apply to the DM-DED group in the current study.
“Regardless, MG loss on its own, which can be directly detected, suggests MG function is surely impaired,” the team explained. “Therefore, these results indicated more severely impaired function of the MG in diabetics with DED than in nondiabetics with DED.”
Significant differences were observed only in the lower eyelid, which consistently worsened as the disease progressed; however, this was not the case in the upper eyelid. This may be caused by the different methods of assessment of MG dropout.
“Alternatively, it indicates that MGD in diabetics may progress earlier in the lower eyelids than the upper eyelids, as there was greater loss of dropout in the lower eyelids compared with the upper lids in the DM and DM-DED groups,” the authors explained. “It is assumed the reason may be attributed to more strongly squeezing the upper eyelids than the lower eyelids during blinking, which induces secretion of meibum more easily and continuously.”
This study also found that the OSDI scores of DM-DED patients were higher than those of the normal controls but lower than nondiabetic DED patients. Similarly, decreased OSDI scores were shown in the DM control group compared with the normal control group, which was consistent with a previous study.
“These findings provide concrete evidence for MGD as related to DM-DED. Nevertheless, it is confusing whether MGD is secondary to DM-DED or the latter is caused by the former,” the authors concluded. “Further study must be performed to reveal the causative link between MGD and DM-DED.”
Yang Q, Liu L, Li J, et al. Evaluation of meibomian gland dysfunction in type 2 diabetes with dry eye disease: a non-randomized controlled trial. BMC Ophthalmol. January 31, 2023. [Epub ahead of print]. |


