 |
|
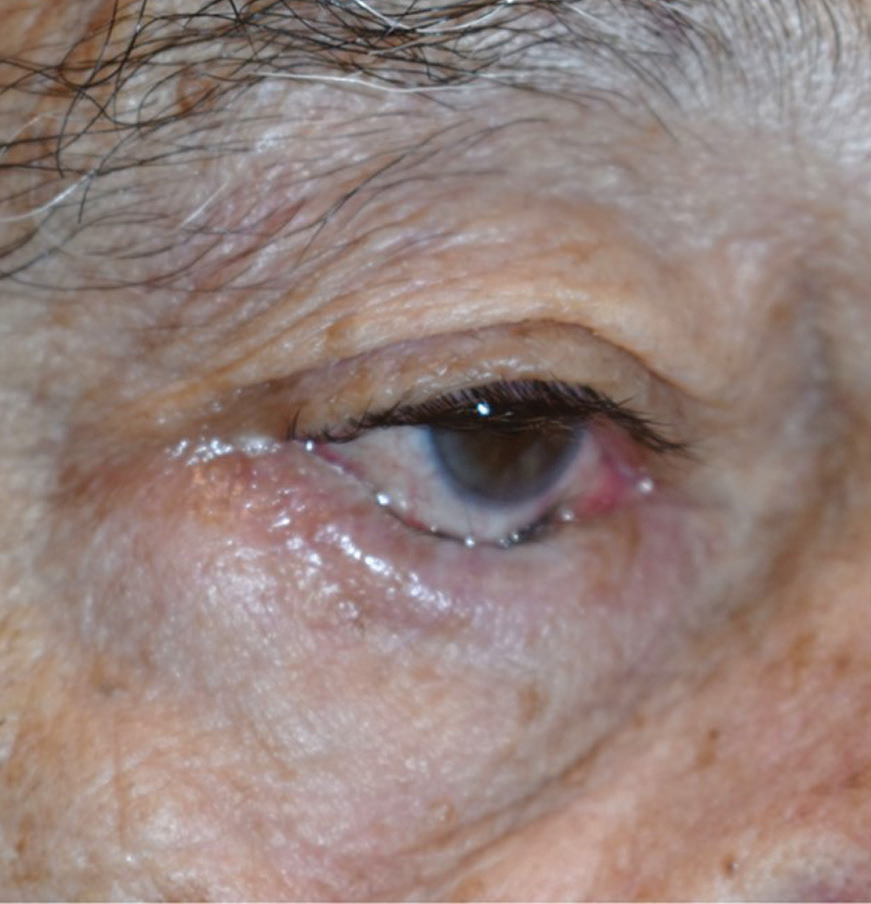
A recent study examined changes in the position of the lower lacrimal punctum and tear meniscus height after addressing horizontal laxity of the lower eyelid in patients with involutional entropion. Photo: Brent Murphy, MD. Click image to enlarge. |
Involutional entropion of the lower eyelid is the most common type, in which the eyelid turns inward due to vertical and horizontal laxities, or looseness. To address the vertical laxity, the eyelid retractor is advanced, while the horizontal laxity is corrected by horizontal tightening or shortening procedures of the eyelid, such as the lateral tarsal strip procedure, transcanthal canthopexy and wedge resection. Researchers recently examined changes in the position of the lower eyelid punctum and tear meniscus height after correction of horizontal laxity of the lower eyelid in involutional lower eyelid entropion. The results of their study imply that lateral shift of the lower lacrimal punctum prevents effective drainage of tears accumulated in the lacrimal lake, resulting in increased tear meniscus height after correcting for horizontal laxity of the lower eyelid in involutional entropion.
This prospective, observational study included 42 sides of 36 patients with involutional entropion who underwent a lateral tarsal strip procedure or transcanthal canthopexy (plus lower eyelid retractor advancement). All measurements were performed preoperatively, at the postoperative third and sixth month.
The lower lacrimal punctum significantly shifted laterally at the three-month follow-up and slightly returned to its original position at the six-month follow-up. Although the differences did not reach statistical significance, tear meniscus height in the lower eyelid increased at three months and then slightly decreased at six.
“A laterally shifted lower lacrimal punctum is, therefore, away from the lacrimal lake, which may interfere with the effective drainage of tears accumulated in the lacrimal lake,” the researchers wrote in their paper.
The study suggested that the lateral tarsal strip procedure secures a tighter fixation, resulting in a more lateral shift of the lower lacrimal punctum and no return of the lower punctum position at the six-month follow-up compared with transcanthal canthopexy. However, the measurement results were not different between patients who underwent either of these surgeries.
“Although we did not evaluate medial and lateral canthal laxities using lateral and medial distraction tests, the Kuhnt-Szymanowski procedure may be a better option to prevent excess lateral shift of the lower lacrimal punctum and following epiphora, particularly in patients with severe laxity of the medial canthus,” the research team wrote.
However, they noted that their study included only Japanese patients. “Since there are known racial differences in eyelid anatomy, the results may not be applicable to other races,” they wrote. “Second, all the measurements
Yokoyama T, Vaidya A, Kono S, et al. Changes in lacrimal punctum position and tear meniscus height after correction of horizontal laxity in involutional lower eyelid entropion. J Ophthalmol. January 17, 2023. [Epub ahead of print]. |


