 |
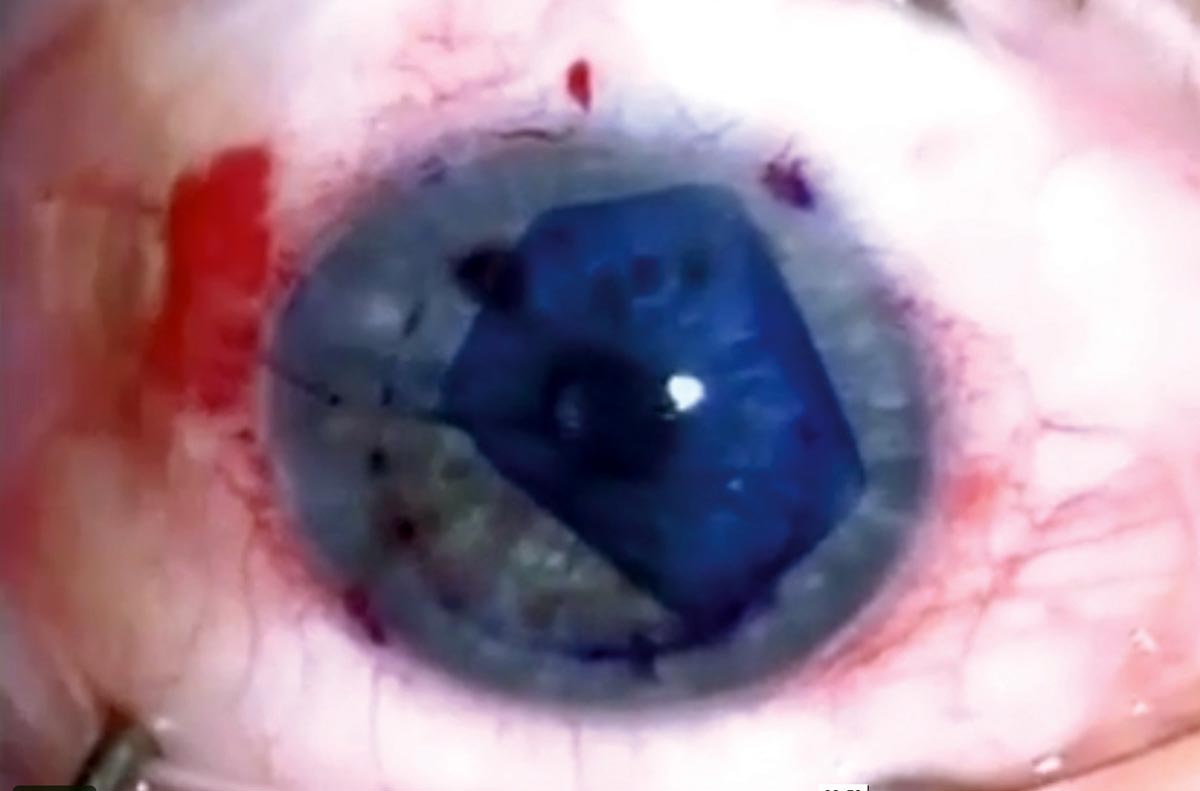
| In a recent study, DMEK (pictured) yielded better post-op visual acuity gains, but one-third of cases required a re-bubbling procedure. Photo: Jim Guzek, MD. Click image to enlarge. |
A new study appearing in Eye had researchers outline a meta-analysis of two versions of endothelial keratoplasty, commonly performed as a treatment for corneal endothelial dysfunction. The newer ultrathin Descemet stripping automated endothelial keratoplasty (UT-DSAEK) and Descemet membrane endothelial keratoplasty (DMEK) were evaluated for their differences in observed best-corrected visual acuity outcomes, endothelial cell density and postoperative complications.
A literature review identified studies that reported comparative results between the two procedures. A total of seven studies were included with analysis of 362 eyes.
The researchers found DMEK to result in better best-corrected visual acuity at the three-month, six-month and one-year marks after operation. However, UT-DSAEK saw a lower total complication rate, at 25.2%, a significantly decreased rate from the 57.3% seen with DMEK. As well, UT-DSAEK resulted in a lower re-bubbling rate (11.0%) compared with DMEK (33.7%). Endothelial cell count did not differ between the two procedure types.
With the difference in visual acuity most pronounced at three months after operation, DMEK’s advantage in this category showcases faster visual rehabilitation for patients and continues this to be significantly better at six months and one year post operation.
The study authors attribute this finding to improved anatomy restoration in this procedure, given the usage of thinner grafts with no lamellae and the absence of stroma-to-stroma graft interface. As the authors explain, thinner grafts induce fewer higher-order aberrations and see less hyperopic shift, thus contributing to its pronounced efficacy in visual acuity over UT-DSAEK. Another consideration here is DMEK’s use of smaller incisions than needed for UT-DSAEK, leading to less surgically induced astigmatism.
DMEK falls short in terms of complications, though, with a higher total complication rate than UT-DSAEK. Most commonly seen for each cohort were instances of graft detachment, requiring re-bubbling. This is a significant concern after DMEK, with an average occurrence rate coming in at just under one-third of patients.
The second most common complication was elevated IOP for each cohort, likely caused by post-op steroid use or, alternatively, developed from air bubble–related pupillary block. Graft failure and rejection were both low, with failure occurring in two DMEK and one UT-DSAEK procedures and rejection in one DMEK and two UT-DSAEK procedures.
With both options presenting their own sets of advantages and challenges, the study authors note that “both procedures remain valuable options for a cornea specialist with prudent decision making given to the right operation for the right patient.”
They end with emphasizing what could not be as easily discerned from their results, highlighting that “large multicenter randomized controlled trials are required to further clarify differences between the two procedures, particularly in terms of endothelial cell loss, graft rejection and overall graft survival.”
Hurley DJ, Murtagh P, Guerin M. Ultrathin Descemet Stripping Automated Endothelial Keratoplasty (UT-DSAEK) vs. Descemet Membrane Endothelial Keratoplasty (DMEK)—a systematic review and meta-analysis. Eye. March 18, 2023. [Epub ahead of print]. |


