 |
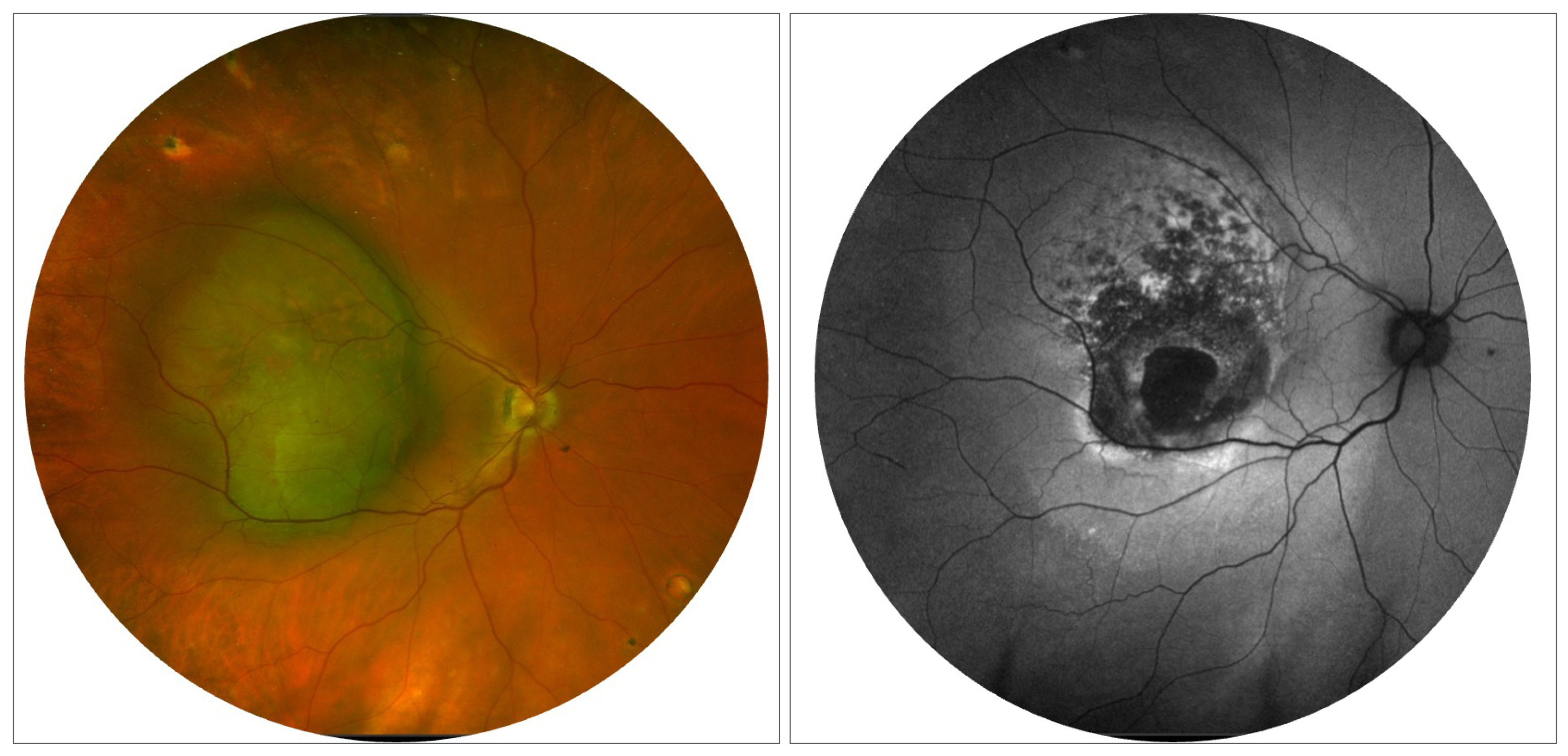
| A recent study proposes that metastases of uveal melanoma could have spread from small tumors during the gap between diagnosis and treatment and remained dormant for a decade before manifesting clinically. Photo:Jessica Haynes, OD. Click image to enlarge. |
The challenge of managing uveal melanoma, the most common primary intraocular cancer in adults, is the unclear prognostic indication of primary tumor treatment. While several tumor characteristics have been linked to increased metastatic risk, the impact of treatment itself is still a subject of debate. If significant delays in primary tumor treatment are associated with a great risk of metastasis, researchers in Sweden wondered if a smaller impact might be possible from the shorter delays typical of standard clinical practice. Their study determined that increasing time between diagnosis and treatment of uveal melanoma was associated with a higher risk of metastatic death. The association was consistent when evaluating prompt treatment (within one month from diagnosis) vs. delayed treatment (≥ one month from diagnosis) in cumulative incidence analyses of patients in American Joint Committee on Cancer (AJCC) stages II and III and in stage I to III combined.
The study, published in Ophthalmology, analyzed a large cohort of 1,145 patients (52% male), examining the correlation between the interval from diagnosis to treatment and the risk of metastatic death. For this study, the date of the uveal melanoma diagnosis—and not the date of discovery of any precursor lesion—was used to determine the time span between diagnosis and treatment. Consequently, the duration a lesion was observed prior to a uveal melanoma diagnosis did not impact the calculated delay times.
Treatment recommendations that were typically made on the day of diagnosis were determined largely by tumor size, location and patient preference. These included:
- tumors ≤16mm in diameter and ≤6mm thick – plaque brachytherapy with ruthenium-106
- tumors ≤16mm in diameter and 6mm to 10mm thick – plaque brachytherapy with iodine-125
- larger tumors – enucleation
The mean interval between diagnosis and treatment was 34 days. Patients treated promptly had larger tumors, but there were no differences in patient age at diagnosis, tumor distance to the optic disc, in rates of ciliary body involvement or extraocular extension or in symptom duration before diagnosis. Those who were treated more than a month after diagnosis had greater uveal melanoma mortality in AJCC stages II and III. In stage I, the uveal melanoma mortality for delayed treatment was lower for the first 10 years, followed by a marked spike in the 11th year.
“It suggests that metastases could have spread from small tumors during the gap between diagnosis and treatment and remained dormant for a decade before manifesting clinically,” the researchers wrote in their paper. “However, our data also indicate that metastases were formed by cells that left larger primary tumors during this gap. Consequently, our results challenge a central concept in the understanding of the metastatic progression in uveal melanoma.”
“In order to explain the strong prognostic implication seen for large tumors treated with a delay, metastatic tumor cells that leave the eye in more advanced stages of the disease had to grow relatively fast, perhaps without the initial period of dormancy that has become a hallmark of this disease,” they added.
In multivariate competing risk regressions of all 1,145 patients with tumor diameter, thickness, ciliary body involvement and extraocular extension as covariates, the risk for mortality increased with 1% for every additional 10-day delay in treatment. Among 355 patients treated with enucleation, this delay was associated with mortality, independent of AJCC stage, cytomorphology and level of immunohistochemical BAP-1 expression.
"While the link between delayed treatment and adverse prognosis was not statistically significant for patients in AJCC stage I alone, it's notable that there was a pronounced surge in uveal melanoma mortality 10 to 11 years post-diagnosis for those receiving delayed treatment in this group,” the study concluded. “These results challenge the prevailing theory of early metastatic seeding in uveal melanoma, emphasize the importance of prompt treatment and merit further validation in independent cohorts with longer follow-up and comprehensive tumor genetic data.”
Stålhammar G. Delays between uveal melanoma diagnosis and treatment increase the risk of metastatic death. Ophthalmology. November 20, 2023. [Epub ahead of print]. |

