 |
|
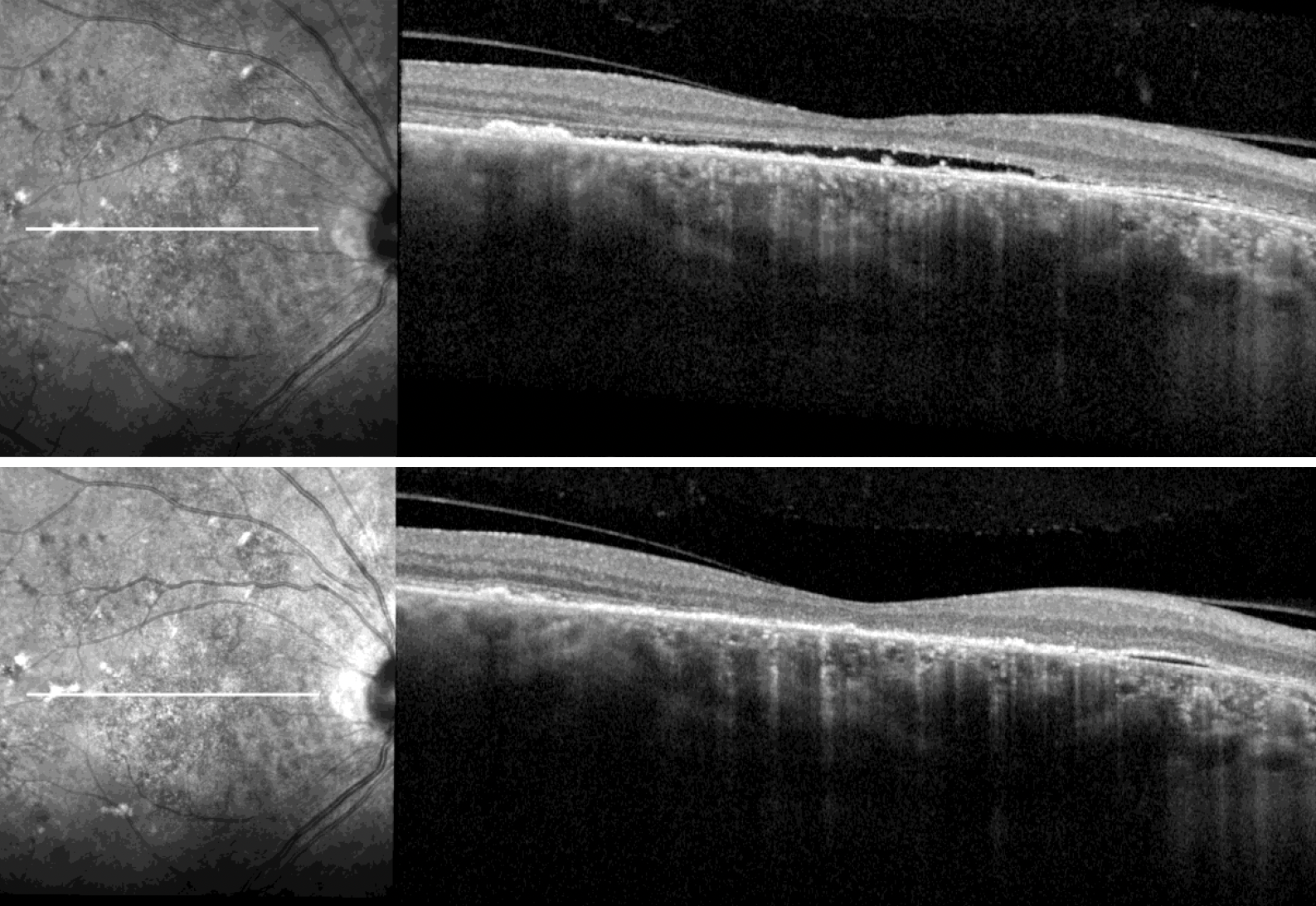
These photos from one subject in the study with chronic CSC show flat subfoveal subretinal fluid at baseline (top) and resolution following treatment with prednisolone eye drops for six weeks (bottom). Increased IOP could be one explanation for the observed reduction, the researchers suggest. Photo: van den Tillaart FM, et al. Retina. March 18, 2024. Click image to enlarge. |
Although the spectrum of pachychoroid conditions comprises many entities, a team of Dutch researchers undertook a new study, published in Retina, that focused on a potential treatment regimen for three loosely related conditions within the category: chronic central serous chorioretinopathy (CSC), pachychoroid pigment epitheliopathy (PPE) and peripapillary pachychoroid syndrome (PPS). The investigation included 54 eyes of 48 patients with one of these diseases, all treated with prednisolone acetate 1% eye drops TID.
On follow-up (mean: 41 days), the 44 eyes with chronic CSC showed significant reduction in retinal central subfield thickness and macular volume; in 22% of these eyes, foveal intra- or subretinal fluid resolved completely. A reduction in the nasal retinal thickness was seen in the eight PPS eyes, while one of two PPE eyes showed structural improvement. None of these diseases displayed significant change in visual acuity.
Overall, anatomical response was observed in the central serous and PPS cases. In those with CSC, complete fluid resolution was seen in 9% of eyes and resolution of foveal fluid occurred in 22% of eyes at follow-up. Although a good response at one month was observed, complete resolution of fluid might have been less common due to a shorter follow-up time. The authors point out the large response of chronic CSC patients in decreased macular volume, occurring in 68%.
Visual acuity was not expected to change, since longstanding presence of subretinal fluid and widespread outer retinal changes were already present at baseline visits of these patients. The study authors also point out that there is a current shortage of verteporfin, thus delaying treatment with photodynamic therapy (PDT) in CSC patients. As the authors argue in their paper, “in the absence of PDT, prednisolone eye drops treatment potentially prevents additional visual loss in a portion of the chronic CSC patients by reducing the duration of subretinal fluid.”
Although the eight cases of PPS did not show significant difference in central retinal thickness, total macular volume or visual acuity, this was likely due to these measures being suboptimal, as fluid in PPS is centered around the optic disc.
Finally, the authors discuss that intraocular pressure (IOP) did increase in SCS patients after the steroid’s use, with 17% of eyes elevating to an IOP >25mm Hg at follow-up; this does not, however, exceed the reported incidence of steroid-induced ocular hypertension in the general population. A nonsignificant IOP was measured in PPS patients as well. Consequently, the researchers caution that “the risk of steroid-induced ocular hypertension is an evident disadvantage of prednisolone eye drops and should be discussed with the patient before initiating treatment.”
From their results, the authors propose that “topical prednisolone eye drops may serve as an alternative treatment for a subset of the non-neovascular pachychoroid related diseases,” adding that the regimen “may serve as a low-cost and easily accessible treatment alternative in countries where PDT is not available at all, of where PDT treatment is not being reimbursed.”
van den Tillaart FM, Temmerman IM, Hartgers F, Yzer S. Prednisolone eye drops as a potential treatment in non-neovascular pachychoroid related disease. Retina. March 18, 2024. [Epub ahead of print]. |


