 |
|
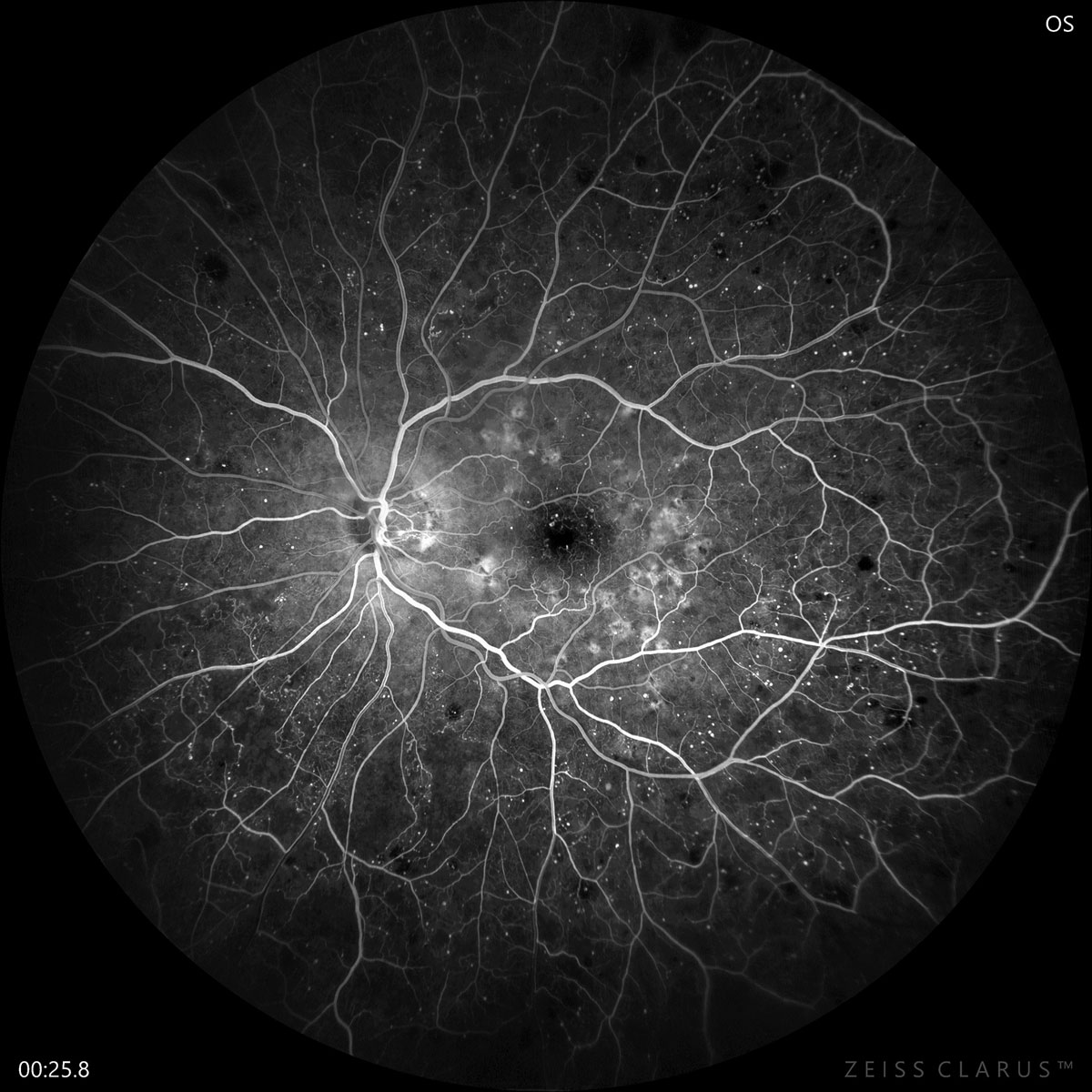
New research again makes the case for the importance of glycemic control in preventing or delaying progression to PDR in diabetic patients. Photo: Jay Haynie, OD. Click image to enlarge. |
A large, five-year longitudinal study analyzing Danish patients recently considered the demographics and clinical characteristics of patients with diabetes to identify factors associated with progression to proliferative diabetic retinopathy (PDR). These patients were then compared to those who did not develop the condition.
Both type 1 and type 2 diabetic patients who attended a national screening program for diabetic retinopathy were included, with a total of 210,945 participants. Diabetic retinopathy was classified through use of The International Clinical Retinopathy Disease Scale (ICRDS), where 0 = no DR, 1 = mild DR, 2 = moderate DR, 3 = severe DR and 4 = PDR.
Progression to PDR was identified in 2,384 eyes of 1,780 patients over the five-year period, equaling 0.9% of the entire cohort. From the baseline diabetic retinopathy level (a rating of 3 on the ICRDS), PDR progression rates at one, three and five years ended up being 3.6%, 10.9% and 14.7%, respectively. Interestingly, the rate of PDR progression from the baseline DR level 3 was lower than previous reports in one, three, and five years out.
Specifically, the researchers of the study look at the Early Treatment Diabetic Retinopathy Study Research Group, which they explain has laid the foundation for developing the International Clinical Retinopathy Disease classification scale also used in this report. This research group found higher progression rates than the current study in all instances, with rates of 17.1%, 44.4% and 57.8% for one-, three- and five-year risk assessment, respectively.
The researchers used a multivariable model to predict the progression of PDR. Factors predicting PDR progression included the duration of diabetes, having type 1 diabetes, a Charlson Comorbidity Index—a measure of the relative one-year risk of mortality based on 17 possible comorbid conditions—score greater than zero, insulin use and anti-hypertensive medication use.
Making this different from similar studies is that, as the researchers put, older studies included diabetic populations that were poorly regulated and high risk. Conversely, this population “contributes new knowledge about the rate of progression in well-controlled patients with diabetes,” as the researchers of the study wrote in their paper for Ophthalmology Science.
The authors of the study point out that current recommendations for screening intervals of patients with DR-level 3 are based on much higher progression rates like that seen in previous studies. What they add is that, as indicated by their results, screening intervals can be reconsidered if all systemic factors are known, including blood pressure and HbA1c level.
Based on this observation, the authors note that “our results strengthen the notion that clinicians should control systemic factors appropriately (HbA1c and blood pressure), treat diabetic macular edema and care for patients in need of special care (pregnancy, bariatric surgery, mental or physical vulnerability) when proposing individual screening intervals.”
Dinesen S, Stokholm L, Subhi Y, et al. Five-year incidence of proliferative diabetic retinopathy and associated risk factors in a nationwide cohort of 201,945 patients with diabetes. Ophthalmol Sci. 2023. [Epub ahead of print]. |


