 |
|
Most forms of hemianopia could potentially help determine poor functional outcome in patients who suffer from acute ischemic stroke. Photo: Carolyn Majcher, OD. Click image to enlarge. |
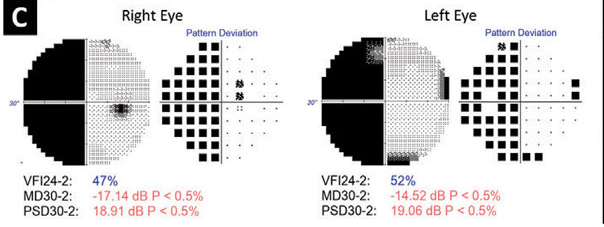
Large vessel occlusion—the obstruction of large, proximal cerebral arteries—has been proved to be an independent predictor for six-month mortality and poor functional outcomes in patients who suffer from acute ischemic stroke. Therefore, rapid detection of large vessel occlusion in patients is essential. A recent study noted that impaired levels of consciousness, visual field loss and sensory loss were independent predictors for large vessel occlusion in mild stroke patients using the National Institutes of Health Stroke Scale (NIHSS). Of the three, visual field loss (which the scale considers partial, complete and bilateral hemianopia) had the highest adjusted odds ratio, 2.10, of predicting mild acute ischemic stroke with large vessel occlusion.
The study collected the data of consecutive patients with acute ischemic stroke with a NIHSS score of five and under from the Third China National Stroke Registry, a prospective nationwide registry of large vessel occlusion or transient ischemic attack patients in China. The NIHSS score consisted of 11 subitems. For each subitem, a score of zero meant normal in this specific function, while a higher score indicated more severe impairment. The scores of each subitem were summed to calculate the NIHSS total score, ranging from zero to 42. Higher NIHSS score s strongly correlated with more severe stroke. Multivariable regression analyses involving clinical characteristics and NIHSS subitems were performed to detect the predictors for large vessel occlusion.
A total of 7,653 patients with mild acute ischemic stroke were included. Among them, 620 patients (8.1%) had an occlusion of anterior and posterior large vessels. Patients with a history of prior transient ischemic attack or stroke, higher NIHSS score and higher admission diastolic were more likely to develop large vessel occlusion. In the subitems of NIHSS score, the researchers found that the level of consciousness (adjusted odds ratio, 1.87), visual field loss (2.10) and sensory loss (0.75) were predictors for mild acute ischemic stroke patients with large vessel occlusion.
In the analysis of the anterior circulation, the dysfunction of sensory, aphasia and motor symptoms was related to infarction in the cortex, which was less commonly found in the subcortical infarction caused by perforator artery occlusion. The higher frequency of visual fields, limb ataxia and level of consciousness in posterior large vessel occlusion patients demonstrated a large infarct in the occipital lobe, cerebellum and brainstem.
Mild acute ischemic stroke patients with large vessel occlusion are more likely to be neglected and not expeditiously treated by recanalization and thrombolysis therapies. The researchers proposed that “further studies are warranted to test these predictors in prehospital settings and in other populations.”
Lu Z, Xiong Y, Yang K, et al. What predicts large vessel occlusion in mild stroke patients? BMC Neurol. 2023;23(1):29. |


