 |
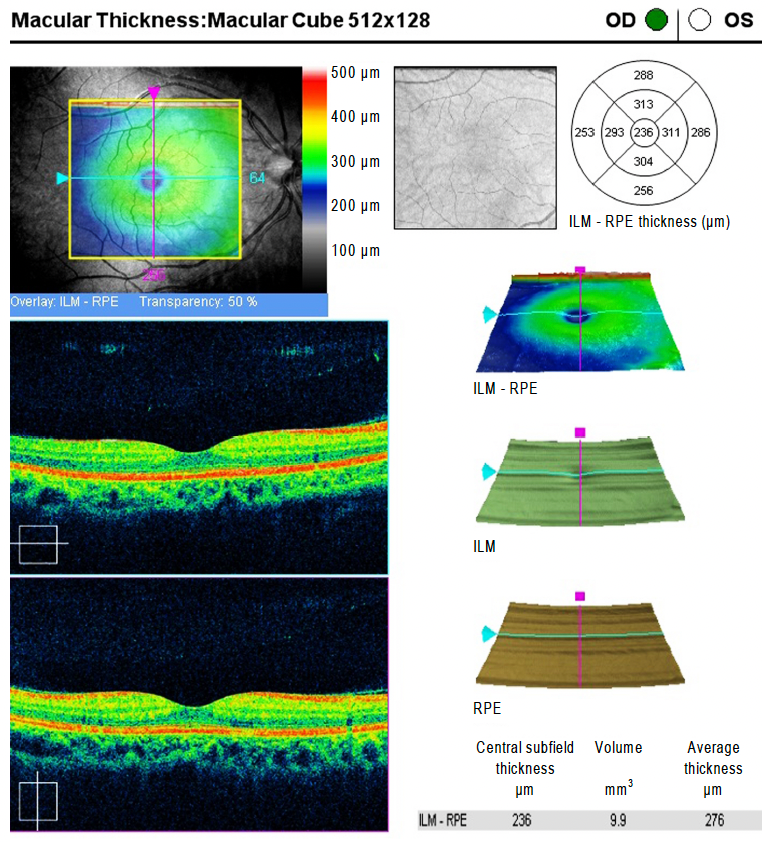
| Retina specialists exhibited the highest level of agreement when grading macular thickness maps of patients with exudative AMD compared with foveal-centered B-scans or five macular B-scans including the central B-scan. (OCT image is from an unaffected patient.) Photo: Kang NH, et al. J Korean Ophthalm Soc. Click image to enlarge. |
Keeping a close eye on macular fluid in patients with exudative age-related macular degeneration (AMD) is crucial to inform treatment decisions and prevent potentially devastating visual outcomes. The declining number of ophthalmologists in the US and the influence of the COVID-19 pandemic are driving the need to come up with at-home monitoring solutions to ensure recurrences are detected in these patients as soon as possible. Findings from a recent study suggest that macular thickness maps alone may be enough to detect recurrent exudation and guide management—even remotely—in those with exudative AMD.
Fifty-three eyes of patients diagnosed with exudative AMD participated in the retrospective, longitudinal study, totaling 1,385 imaging sessions using macula-centered 6x6mm OCT scans. In each case, five retina specialists (graders) were asked to determine if there were changes that warranted a full clinical assessment after viewing two scans using one of three different imaging strategies: macular thickness maps alone, individual foveal-centered B-scans alone or five macular B-scans including the foveal-centered B-scan.
The level of agreement among graders was greater than 80% across the board. The Fleiss kappa—a statistical measure for assessing the reliability of agreement—was highest when graders were given macular thickness maps alone compared with the ground truth. Additionally, when the averages of all five graders were compared with the ground truth, the macular thickness maps alone showed the highest level of agreement (90.05%) followed by the central B-scans (87.87%) and the five B-scan method (86.51%).
“Compared with the gold standard of reviewing the entire OCT scan at a review station, we found that reviewing the macular thickness maps alone was almost as good at identifying recurrent exudation at the review station, and certainly as good, if not better, than reviewing a central macular B-scan or the five-line B-scan cluster for deciding if an immediate office assessment was warranted,” the researchers explained in their paper, published in American Journal of Ophthalmology. “While these data were collected in a clinical setting, the results strongly suggest that if similar quality scans were obtained in a remote setting, then the macular thickness maps alone would be sufficient to make the decision to bring the patient in for a likely treatment,” they concluded.
Trivizki O, Varcheie M, Bello S, et al. Assessing change in exudative AMD with macular thickness maps as a surrogate strategy for remote patient monitoring. Am J Ophthalmol. July 25, 2023. [Epub ahead of print]. |

