 |
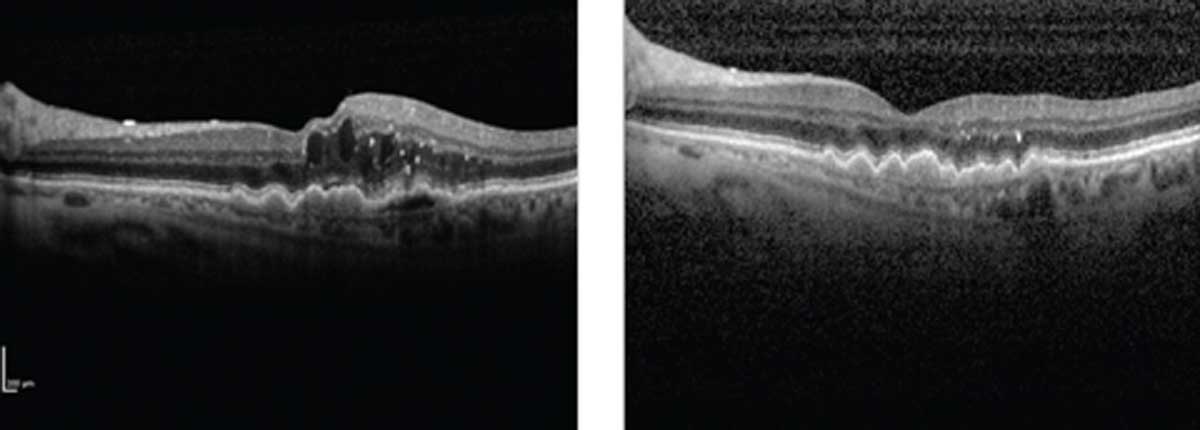
Depending on where the neovascular lesion was located, visual acuity outcomes were detected among the nAMD patient cohort in this study. Photo: Nat Loewenstein, MD. Click image to enlarge. |
Anatomic classifications for neovascular lesions have been shown to be tied to visual acuity in patients with neovascular age-related macular degeneration (nAMD), a leading cause of severe vision loss in those older than 50. A greater understanding of the disease’s pathophysiology is warranted to be able to recommend a more individualized treatment course to these patients.
A study group called the Consensus on Neovascular Age-Related Macular Degeneration Nomenclature (CONAN) recently published a consensus on the need to classify nAMD subtypes using aspects of multimodal imaging. The group characterized the types of neovascularization into four classes based on the anatomic location of the lesion: type 1, type 2, mixed types 1 and 2 (type 2/M) and type 3.
To determine whether these classifications were associated with visual acuity outcomes in nAMD patients, the researchers performed a post-hoc analysis on Phase III of HARBOR, a 24-month trial of ranibizumab in patients with nAMD. They analyzed baseline imaging data, macular neovascularization (MNV), subretinal and/or intraretinal fluid and spectral domain OCT images through month 24. Then, they compared the change in mean best-corrected visual acuity (BCVA) over time and at months 12 and 24.
Of the 700 study eyes included, 37.6%, 41% and 21.4% eyes had type 1, type 2/M and type 3 lesions at baseline, respectively. Type 1 eyes were found to have the best mean BCVA both at baseline and at month 24, while type 2/M eyes had the worst. By month 24, type 2/M eyes had the most significant gain in BCVA, and patients with types 1 or 3 showed similar improvement.
“In this first application of CONAN Study Group criteria to a major nAMD dataset, we showed that baseline MNV lesion type correlated with 24-month vision outcomes among ranibizumab-treated eyes in the Phase III HARBOR trial,” the study authors concluded. “Type 2/M lesions had the lowest BCVA overall but achieved greater mean vision gains at months 12 and 24.” They added that the results also suggest “eyes with type 1 MNV at baseline are more likely to maintain greater visual acuity over time.”
The association between baseline MNV lesion type and vision outcomes is evident from the data and suggests a need to develop an anatomic MNV classification system that can be used to “characterize the diversity seen among patients with nAMD and prognosticate visual responses to anti-VEGF therapy in clinical practice.”
Freund KB, Staurenghi G, Jung JJ, et al. Macular neovascularization lesion type and vision outcomes in neovascular age-related macular degeneration: post hoc analysis of HARBOR. Graefes Arch Clin Exp Ophthalmol. March 3, 2022. [Epub ahead of print]. |


