 |
The most crucial aspect of any examination is the history. A comprehensive history includes talking with the patient and getting to know them. Not only do you foster a relationship that will hopefully last for years to come, but you can also better serve the patient’s needs as well. You might learn that a patient is struggling in school and suggest a referral to a learning specialist or neuropsychologist or run a few extra binocular vision tests. You may learn that a patient recently lost a family member and extend condolences and a listening ear; if needed, you can provide a referral to a counselor. You could learn that a patient has not had a physical in many years and suggest visiting their primary care physician.
The list of things is literally endless and can ultimately help you decide on the best course of action for each of your patient’s visual needs. We will use the following three cases to help illustrate and drive home this crucial point:
Case 1
A 19-year-old male presented for a routine exam complaining of intermittent blur at distance. His VA was 20/25 OD, 20/20- OS and 20/20 OU at distance and 20/25 OD, OS and OU at near. His stereo was 70 seconds, cover testing was ortho at distance and near, NPC was reduced at 14cm break and 17cm recovery and the rest of the chair skills were normal. His dynamic retinoscopy and refraction showed values of -0.50 -0.25x090 OD and -0.25 -0.25x090 OS. The NRA/PRA was +2.25/-1.75.
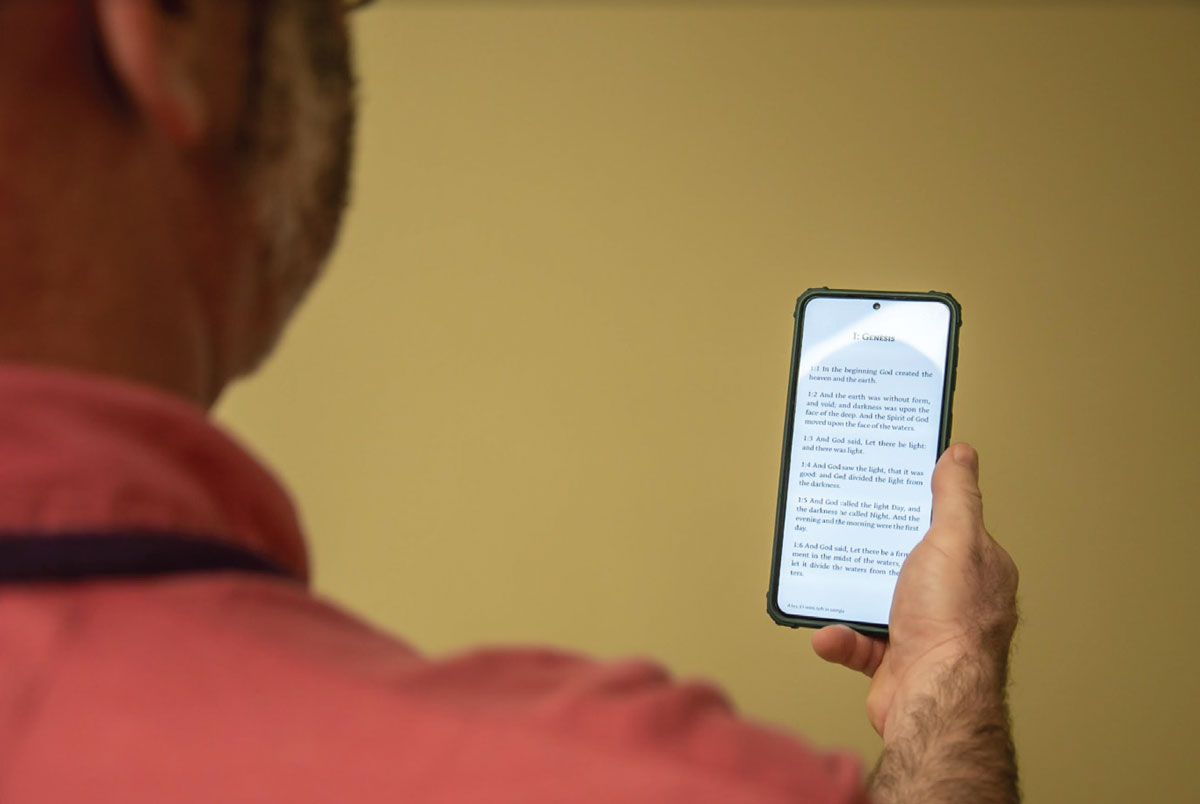
The student quickly realized that this was an accommodative issue due to the data and the answers to questions about his current visual needs. Simply inquiring about what he was doing for work and school opened up a treasure trove of helpful information. He was in ministry and spent significant time reading the Bible on his phone and using the computer. Plus at near (+0.75 OU) was trial-framed at near. His stereo and NPC both improved with the plus in place. He was prescribed near vision-only glasses to be used with reading and computer work.
Case 2
A 21-year-old female presented with a history of wearing +0.75 reading glasses prescribed two years prior. The glasses worked for a short period of time, but then the patient saw double. Her VA was 20/25 OD, OS and OU at distance and 20/25 OD, OS and OU at near without the glasses, which improved to 20/20 at distance and 20/20- at near with the glasses. The stereo was 25 seconds, cover testing was ortho at distance and 8pd exophoria at near, NPC was reduced at 14cm break and 19cm recovery and the rest of the chair skills were normal. The near vergence ranges were 10/18/7 base-in and 12/20/4 base-out.
It was clear that the patient needed to continue using the plus at near, but vision therapy was needed for true relief. The path to the ultimate treatment came from the history and questioning about work and school. She was a full-time daycare worker, and she was doing online schooling. Coming in for vision therapy was not in the cards due to her limited free time during the day. The remaining tool on our belt was prism at near, so we trialed 3pd base-in. The patient noticed the change immediately, reporting that “things seemed so much clearer.” She was once again prescribed near vision-only glasses, but this time we added 1.5pd base-in to each eye. For this patient, knowing about her work/school balance and what would work best for her helped direct our treatment path.
 |
|
Near-point issues occur with or without the use of technology such as the smartphone. Click image to enlarge. |
Case 3
A 52-year-old male presented four months post-stroke, complaining of constant double vision. Another clinician originally saw him in a rehab facility. His cover test showed 30pd exophoria and 4pd left hyperphoria, but prism neutralization proved unsuccessful. He was prescribed spot occlusion, as the double vision could not be resolved. Several months later, the cover test now showed 15pd exophoria and 4pd left hyperphoria, but once again, the double vision was not correctable, returning after one to two minutes.
At the current visit, VA with his flat-top bifocal was 20/20 OD, OS and OU at distance and 20/30 OD, OS and OU at near. His eye movements were atrocious: pursuits were jerky and labored, and saccades were inaccurate, with under- and over-shooting. The cover test now showed 8pd exophoria and 4pd left hyperphoria. We again attempted to neutralize the double vision but were thwarted; after several minutes, it returned at distance.
Typically, if there is significant fluctuation in the stability of the visual system, we refrain from grinding in prism. Still, we took into account that the patient was a lawyer who typically performed a significant amount of near work. He desired to read again but was hampered by double vision. Reading was not only needed for work; it represented normalcy and freedom for him.
Since we typically take brain-injured patients out of their multifocal lenses, we prescribed near vision–only glasses with horizontal and vertical prism ground in. We showed caution by trial-framing the potential prescription with 2pd base-in OD and OS and 2pd base-down OS and having the patient read for 10 to 15 minutes. Luckily, the double vision did not return.
Discussion
A good history includes more than just a rundown of visual symptoms. We ask about medical and visual history, developmental history, academics, sports, hobbies and work. These do not just check boxes on the screen; we use the info we gather to help make important care-related decisions.
As you can see in the three included cases, the fact that the patients were students, how much they worked at near, whether they could attend vision therapy and what kind of work they did all made a difference in our treatment approach. Even though we are all rushed to see more patients in a given timeframe, we have to stop and smell the roses and actually talk to them. Doing so will not only help us as doctors but will also help our patients achieve a higher quality of life in whatever they choose to pursue.
Dr. Taub is a professor, chief of the Vision Therapy and Rehabilitation service and co-supervisor of the Vision Therapy and Pediatrics residency at Southern College of Optometry (SCO) in Memphis. He specializes in vision therapy, pediatrics and brain injury. Dr. Schnell is an associate professor at SCO and teaches courses on ocular motility and vision therapy. She works in the pediatric and vision therapy clinics and is co-supervisor of the Vision Therapy and Pediatrics residency. Her clinical interests include infant and toddler eye care, vision therapy, visual development and the treatment and management of special populations. They have no financial interests to disclose.

