 |
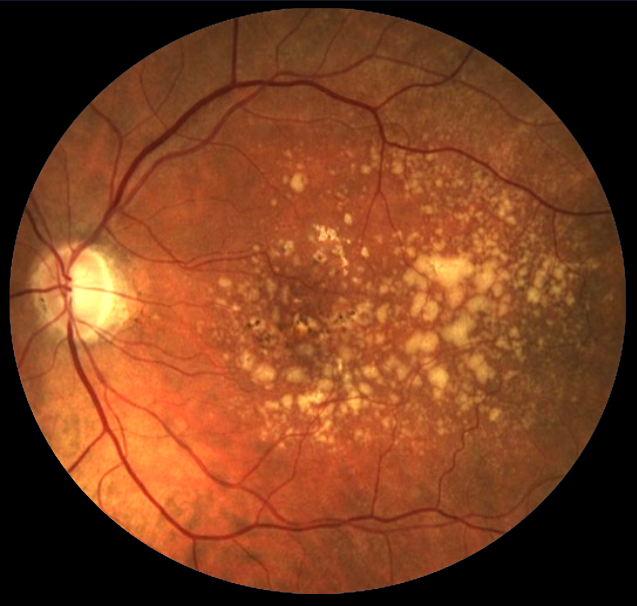
| The prevalence of AMD among US Medicare beneficiaries is approaching two million individuals, study finds. Photo: NEI. Click image to enlarge. |
The number of older adults in the US is increasing precipitously and the Medicare ranks are likely to increase as well. A team of American researchers recently decided to provide updated data on the diagnosed prevalence and incidence of major chronic age-related eye diseases in Medicare fee-for-service beneficiaries. Their analysis over a 15-year period determined that, compared with older epidemiological estimates from 30 years ago, the diagnosed prevalences of AMD, diabetic retinopathy (DR) and glaucoma studied were all higher in more recent years.
The study, published in Ophthalmology, assessed Medicare beneficiaries aged 68 and older from 2005 to 2020. At baseline, in 2005, 60% of included beneficiaries were female, 20% were aged ≥85, 86% were non-Hispanic Caucasian and about 25% had diabetes.
During the non-COVID study period, from 2005 to 2019, the overall diagnosed prevalence of one or more chronic, age-related eye disease increased by 2.9%, from 15.0% (n=3,312,812) to 17.9% (n=3,731,281). Diagnosed incidence decreased over this period from 4.7% (n=917,846) in 2005 to 4.2% in 2019 (n=757,696).
Observing each disease individually, prevalence of AMD increased from 6.8% (n=1,504,770) to 9.4% (n=1,965,176). The researchers propose that one possible explanation is that a greater proportion of newly eligible Medicare beneficiaries carry a prevalent diagnosis of AMD.
“Increased use of OCT in recent decades may also have led to the diagnosis of AMD at a younger age in those with early drusen or pigment epithelial abnormalities that may have otherwise be overlooked on fundoscopic examination,” they wrote in their paper.
The diagnosed prevalence of any DR among those with diabetes decreased from 9.3% (n= 504,135) to 9.0% (n=532,859); however, the diagnosed prevalence of vision-threatening DR increased from 2.0% to 3.4%. The research team noted that, “the increase in the diagnosed prevalence of vision-threatening DR could also be related to greater use of eyecare services, as those under frequent care may be more likely receive this diagnosis.”
Lastly, the diagnosed prevalence of any diagnosed glaucoma decreased from 8.8% (n= 1,951,141) to 8.1% (n= 1,692,837).
Hispanic beneficiaries had the highest diagnosed incidence throughout the study period, and by 2019 also had the highest diagnosed prevalence of DR of all ethnic/racial groups. The researchers emphasized that, specifically, Hispanic and non-Hispanic Black individuals were less likely to receive eye care and are at disproportionately high risk for DR and glaucoma, so true prevalence and incidence differences between racial and ethnic groups may be greater than they had reported.
Unsurprisingly, the diagnosed prevalence and incidence of each condition examined in the study decreased in 2020 compared with preceding years. The researchers proposed that “there may be a large number of incident cases of age-related eye diseases that were undiagnosed during that year, which may increase future incidence rates and disease severity at the time of presentation.”
The team concluded that they hoped that “their findings may inform public health and policy planning and resource allocation to address the eye health of an increasingly older US population.”
Ehrlich JR, Andes LJ, Eisenberg A, et al. Trends in the diagnosed prevalence and incidence of major eye diseases in Medicare Part B fee-for-service beneficiaries aged 68 years or older. Ophthalmology. July 24, 2023. [Epub ahead of print]. |

