 |
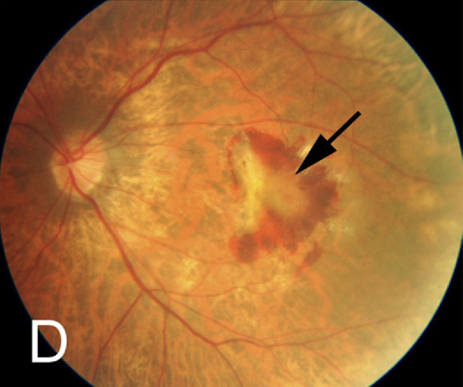
| Impaired VEGF upregulation may explain why older patients had a lower risk of second-eye myopic macular neovascularization (MNV) onset than patients under 40. Photo: Julie Poteet, OD. Click image to enlarge. |
As the number of myopes and high myopes around the world grows, eyecare providers will need to be on high alert for related sight-threatening conditions. Myopic macular neovascularization (MNV), a complication of high myopia, often leads to sudden, progressive visual acuity decline. Anti-VEGF injections can offer short-term visual improvement for affected patients, but early diagnosis is vital to preserving vision and decreasing the recurrence rate.
Recently, researchers investigated the incidence of second-eye involvement after myopic MNV onset and identified clinical risk factors in Europeans. Their results, published in Ophthalmology Retina, demonstrated similar incidence rates to those seen in Asian studies, prompting the authors to recommend close monitoring and increased awareness, especially in younger patients.
The researchers retrospectively analyzed 13-year data of 88 patients (mean age 57) with high myopia (mean axial length 30mm, SE -14D) at baseline. During the follow-up period, 27% of fellow eyes developed myopic MNV, demonstrating an incidence rate of 4.6 per 100 person years, with cumulative incidences of 8%, 21% and 38% at two, five and 10 years, respectively.
On average, MNV developed in the fellow eye after 48 months. The researchers noted that patients under 40 at initial presentation had a 3.8x higher risk of developing bilateral myopic MNV.
Lacquer cracks in the second eye seemed to increase risk for onset, but this risk factor couldn’t be confirmed in the study. A previous study reported similarities between first-eye and second-eye phenotypes.
“Current insights are that European and Asian patients show a similar myopic phenotype, with age and axial length as the most important drivers for myopic maculopathy,” the researchers wrote in their paper for Ophthalmology Retina. “Also, the genetic drivers of refractive error appear to be highly correlated between European and Asian individuals. Taking these parallels together, it is valid to assume that the risk and presentation of myopic MNV for first and second eyes of highly myopic patients is not determined by ethnicity.”
They concluded that close monitoring and immediate treatment upon identification of symptoms will “create an optimal starting point for saving sight in highly myopic patients.”
Ravenstijn M, Klaver CCW, Yzer S. Incidence and risk factors of second eye involvement in myopic macular neovascularization. Ophthalmology Retina 2023. [Epub ahead of print]. |

