 |
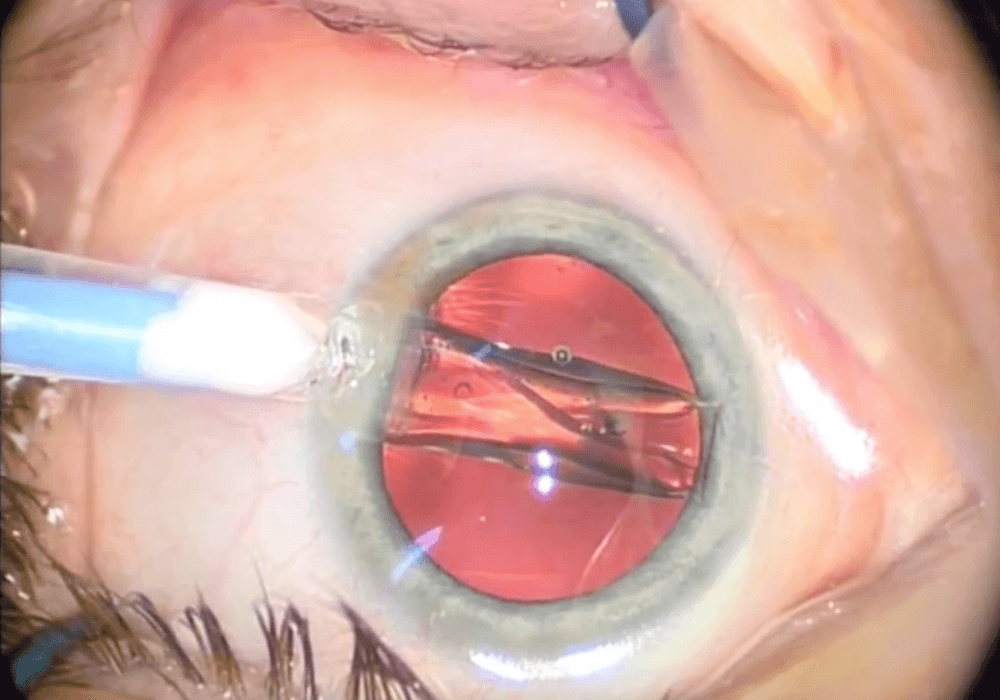
| Reducing a cataract patient’s post-op treatment regimen to one eye drop (an NSAID, in this case) by injecting the other two medications can ease the individual’s recovery and reduce the likelihood of compliance problems. This study found most outcomes as good or better than triple-drop therapy. Photo: Christine Sindt, OD. Click image to enlarge. |
After surgery to remove cataracts, surgeons routinely use topical medications to prevent infections and inflammation. However, the typical regimen of topical antibiotics, corticosteroids and a nonsteroidal anti-inflammatory (NSAID), also known as “triple-drop therapy” (TDT), comes with its own set of limitations, including cost, patient adherence issues and the potential for elderly patients to experience physical difficulty administering drops. Due to these factors, alternatives have emerged. While perioperative intracameral injection is quite popular with cataract surgeons, a group of researchers decided to investigate outcomes with intravitreal administration of an antibiotic and a steroid (abbreviated IVAS) coupled with post-op topical NSAID, a regimen known as IVAS-NSAID for short. The antibiotic agent was moxifloxacin and the steroid was triamcinolone.
The retrospective study compared non-infectious outcomes of this method against topical therapy usage. In total, 2,143 eyes of 2,143 patients—1,079 receiving IVAS-NSAID and 1,064 receiving TDT—who underwent cataract surgery were included from three diverse study centers in the US. Best-corrected visual acuity and intraocular pressures (IOP) were similar between the groups at all time points of one week, one month and six months post-surgery.
A total of 11.6% of TDT eyes developed post-op complications, but the rate was even lower in the IVAS-NSAID group—just 6.5%. Interestingly, both patients who underwent femtosecond laser–assisted cataract surgery (FLACS) and those with dark irides experienced a higher incidence of persistent corneal edema after IVAS-NSAID. As well, those with dark irides also saw higher incidence of cystoid macular edema and rebound inflammation.
Expanding on these findings, the study authors explained, in a paper for American Journal of Ophthalmology, that “IVAS-NSAID may be considered a safe alternative to topical regimens in non-FLACS and light irides patient populations” while reducing the eye drop burden for most patients.
Similar rates of IOP elevation were seen between both groups, which could be explained for a few reasons. One is that surgeons used a technique of manual wound burping after IVAS injection to confirm acceptable IOP, which was not routinely done in the TDT group. Another likelihood is due to the researchers of this study using lower concentration of triamcinolone (2.25mg) in the IVAS injection than what is injected for posterior segment inflammation (4mg), which has been the focus of previous studies that reported higher IOP rates with injection. As well, injection closer to the limbus carries greater propensity for IOP elevation.
Post-op inflammatory events were similar, with risk factors of particular concern (prior uveitis, diabetic status) not associated with increased inflammatory risks with IVAS-NSAID; this demonstrates a comparable safety profile to TDT without posing additional risks, the researchers said.
Patients who underwent FLACS and received IVAS-NSAID had higher rates of persistent corneal edema, reflecting previous reports citing increased post-op inflammation following FLACS. Similarly, those with dark irides have previously been found to have higher rates and degrees of postoperative inflammation, reflecting the greater rates seen in this study of rebound inflammation, persistent corneal edema and cystoid macular edema.
Due to this association, the researchers suggested that “surgeons may consider avoiding IVAS in patients with dark irides or using additional anti-inflammatory medications (e.g., additional injectable, implantable or topical steroids) to supplement IVAS-NSAID.”
Other than these contraindications, the IVAS-NSAID technique may improve patient compliance and reduce healthcare costs while providing a simplified post-op medication course, the researchers concluded, stating their belief that “these findings can aid surgeons in developing personalized postoperative regimens for the optimal use of IVAS-NSAID, based on patients’ comorbidities and demographic characteristics.”
Mian OT, Asif H, Sandhu U, et al. Non-infectious outcomes of intravitreal antibiotic-steroid injection and topical NSAID vs. triple drop therapy post cataract surgery. Am J Ophthalmol. November 7, 2023. [Epub ahead of print]. |

