Rheumatoid arthritis (RA), a chronic, progressive inflammatory disease that results in many ocular complications, affects approximately 1% of the adult population in the United States.1 Certain Asian populations have a slightly lower prevalence, while certain Native American populations have a higher prevalence.1
RA belongs to the same autoimmune disease category as psoriatic arthritis, juvenile polyarthritis, human parvovirus B19, systemic lupus erythematosus and palindromic arthritis. RA can afflict patients of any age, but it typically occurs in patients between 40 to 70 years old. Disease prevalence is 2.5 times greater in women than in men.2
Etiology
Although the specific etiology of RA is unknown, one current theory suggests a genetic predisposition in which an unknown trigger (perhaps several) initiates multiple genes. Studies have shown a concordance rate of 15% to 30% in monozygotic twins and that monozygotic twins are 3.5 times more likely to develop RA than dizygotic twins.2 However, familial aggregation is reported less frequently for RA than for other autoimmune diseases, such as systemic lupus erythematosus (SLE) and multiple sclerosis (MS).
Another theory: RA may be associated with female sex hormones. This theory considers the increased prevalence of RA in women, remission during pregnancy and the increased risk of RA postpartum.3
Autoimmune diseasessuch as RA, Graves disease, MS, SLE, giant cell arteritis and Sjgrens syndromeoccur when the patients immune system mistakenly attacks tissues of the body. Lymphocytes initiate the destructive immune cascade by producing cytokines, which cause damage and inflammation. The cytokines may take the form of tumor necrosis factor alpha (TNF-a), granulocyte-macrophage colony-stimulating factor or various interleukins.
The synovial membranes and articular structures of the joints are the primary targets of the abnormal immune response in RA. Common extra-articular manifestations include rheumatoid nodules, ocular disease, Sjgrens syndrome, rheumatoid vasculitis and neurological disease. Although females have a significantly greater predilection for RA and Sjgrens syndrome, the extra-articular manifestations are more commonly observed in males (figure 1).4
 |
|
1. This patient, who has both rheumatoid arthritis and secondary Sjgrens syndrome, has joint deformity. |
The onset of RA is usually insidious over a period of weeks to months. RA progresses from swelling of the synovial lining to synovial thickening and, eventually, deformity of the joints. A diagnosis of RA is based on a patients medical history, physical examination, serology and imaging studies.
Common symptoms of RA include symmetrical stiffness in multiple joints, morning stiffness in the joints for more than one hour and generalized fatigue. Clinical signs of RA include joint swelling and tenderness.
Serologic testing, which is commonly performed when RA is suspected, consists of the following:5
Complete blood count (CBC). The CBC shows normochromic-normocytic anemia in 80% of cases.
Erythrocyte sedimentation rate (ESR) and C-reactive protein. An elevated ESR occurs in 90% of cases. Both the ESR and C-reactive protein measure inflammation, but a more immediate response occurs in the C-reactive protein when inflammation increases or decreases.
Rheumatoid factor (RF). A positive RF occurs in approximately 70% of rheumatoid arthritis cases.
The earliest radiographic change noted is soft tissue swelling followed by uniform joint-space narrowing. The anti-cyclic citrullinated peptide (anti-CP) ELISA (enzyme-linked immunosorbent assay) is a new test that may help physicians diagnose RA earlier.6 A more aggressive disease course has been found in patients with anti-CP at diagnosis, despite anti-rheumatic treatment, but the test was not found to be beneficial when monitoring disease activity.7
|
Table 1: 1987 Criteria for the Classification of Rheumatoid Arthritis |
|
Criterion |
Definition |
| 1. Morning stiffness | Morning stiffness in and around the joints, lasting at least one hour before maximal improvement. |
|
2. Arthritis of three or more joint areas |
At least three joint areas simultaneously have had soft tissue swelling or fluid (not bony overgrowth alone). The 14 possible areas are the right or left proximal interphalangeal joint, metacarpophalangeal joint, wrist, elbow, knee, ankle and metatarsophalangeal joints. |
| 3. Arthritis of hand joints | At least one area swollen (as defined in #2) in a wrist, metacarpophalangeal joint or proximal interphalangeal joint. |
| 4. Symmetric arthritis | Simultaneous involvement of the same joint areas (as defined in #2) on both sides of the body (bilateral involvement of proximal interphalangeal joints, metacarpophalangeal joints or metatarsophalangeal joints is acceptable without absolute symmetry). |
| 5. Rheumatoid nodules | Subcutaneous nodules, over bony prominences or extensor surfaces or in juxta-articular regions. |
| 6. Serum rheumatoid factor | Demonstration of abnormal amounts of serum rheumatoid factor by any method for which the result has been positive in <5% of normal control subjects. |
| 7. Radiographic changes | Radiographic changes typical of rheumatoid arthritis on posteroanterior hand and wrist radiographs. These must include erosions or unequivocal bony decalcification localized in or most marked adjacent to the involved joints. Osteoarthritis changes alone do not qualify. |
|
Source: Arnett FC, Edworthy SM, Bloch DA, et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum 1988 Mar;31(3):315-24. |
Treatment
Structural damage can develop in the first two years of RA onset.8 Therefore, aggressive treatment to reduce inflammation should be initiated to prevent damage to and deformity of the joints. Therapy should depend on each patient and disease severity. Treatment of RA should involve a combination of patient education, rest, exercise, medications, joint protection and surgery.
Nonsteroidal anti-inflammatory drugs (NSAIDs) and corticosteroids have long been used as first-line medications to control symptoms. Second-line medications include disease-modifying anti-rheumatic drugs (DMARDs) and biologic response modifiers (BRMs). DMARDs suppress the immune system and inhibit the loss of cartilage and bone, and BRMs influence cytokine activity. Even with the release of Rheumatrex (methotrexate, Stada Pharmaceuticals), Plaquenil (hydroxychloroquine, Sanofi-Synthelabo) is the most common DMARD we use in our practice.
Corticosteroids and hydroxychloroquine may cause both systemic and ocular side effects. Corticosteroids can cause dizziness, nausea, weight gain, fatigue, puffing of the face, swelling of the ankles and feet, mood changes and sleep disturbances. They can also cause increased susceptibility to infections and bone fractures. The major ocular side effects of oral corticosteroids are posterior subcapsular cataracts and elevated IOP.
Hydroxychloroquine can cause gastrointestinal side effects and ocular toxicity. Ocular toxicity can take the form of maculopathy, keratopathy or diplopia.9 Maculopathy can cause irreversible central vision loss, although this rarely occurs. If your patient takes hydroxychloroquine, take a complete history of the duration of treatment and dosage. Also, perform color vision testing, photodocumentation of the macula and automated perimetry of central vision (e.g., Humphrey central 10-2) every six months to one year. Although white-on-white automated visual field testing is less sensitive than other testing strategies, we believe the increased reliability allows us to make better clinical decisions.
Ocular Manifestations of RA
Approximately 25% of patients who have RA will report ocular manifestations.9 Keratoconjunctivitis sicca (KCS), episcleritis, scleritis, keratitis and peripheral corneal ulceration are common. Retinal detachment, choroiditis, episcleral nodules, retinal vasculitis and cystoid macular edema have also been reported in association with RA.10 One retrospective chart review study reported a 10.8% incidence of episcleritis in RA patients and a 17.5% incidence of scleritis in RA patients.11 Sjgrens syndrome occurs in 10% to 15% of RA patients.4 RA can also affect other exocrine glands and cause decreased perspiration, dry skin, dry nose and dysphagia.
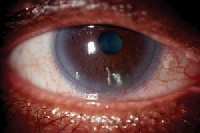
Keratoconjunctivitis sicca. KCS, the most common ocular manifestation of RA, occurs in 15% to 25% of RA patientseither independently or in association with Sjgrens syndrome (figure 2).12,13 This is due to lacrimal gland inflammation and meibomian gland dysfunction (MGD). Biomicroscopic findings include a diminished tear meniscus, intrapalpebral corneal staining with sodium fluorescein and/or lissamine green, decreased tear breakup time and a Schirmer test result of 10mm or less.
 |
|
2. This patient has keratoconjunctivitis sicca with filamentary keratitis. |
Medical therapy may involve topical Restasis (cyclosporine A, Allergan) and/or oral Minocin (minocycline, Wyeth). You may need to educate the comanaging rheumatologist that liver enzymes do not need to be monitored when patients use topical cyclosporine A. Consult a rheumatologist when considering minocycline for MGD because minocycline is also being studied as a systemic treatment of RA. Omega-3 essential fatty acid supplements, derived from various fish and plant sources, may alleviate dry eye symptoms by decreasing prostaglandin production.
Filamentary keratitis often accompanies KCS. We primarily treat this condition by physically removing the strands. A mucolytic preparation, such as 5% acetylcysteine, may help dissolve the filaments in situ. However, this formulation is not commercially available and may be difficult for patients to obtain. Therapeutic contact lenses can also be used to treat patients who have recalcitrant filamentary keratitis. Currently, the use of punctal occlusion for dry eye associated with RA is controversial because of the inflammatory component of RA.
 |
|
3. This patient with diffuse episcleritis shows red, episcleral injection. |
 |
|
4. Notice the nodule in this patient who has nodular episcleritis. |
Scleritis is inflammation of the sclera and includes the presence of scleral edema. Scleritis may manifest in several forms, including diffuse (figures 5 and 6), nodular, necrotizing or posterior.
 |
 |
|
5, 6. The diffuse scleritis in this patient has a purplish hue. |
The following are common differences between scleritis and episcleritis:
The hue of hyperemia is generally pink to red with episcleritis, and blue to purplish-red with scleritis.
Hyperemia usually blanches with topical phenylephrine in patients who have episcleritis but not in those who have scleritis.
Palpation of the globe often elicits marked tenderness in patients who have scleritis, but generally not in those who have episcleritis.
Scleral edema is present in scleritis but absent in episcleritis. Scleral edema may be viewed with a narrow slit lamp beam (optic section/parallelepiped) after applying topical phenylephrine. It will manifest as a bowing of the beam along the sclera.14
Scleritis can be associated with uveitis and peripheral ulcerative keratitis, but these conditions also may occur independently.
Posterior scleritis, which is best diagnosed with ultrasonography, is usually associated with a concurrent anterior scleritis.
|
Table 2: Is it Scleritis or Episcleritis? |
| Variable | Scleritis |
Episcleritis |
| Hyperemia |
Hue is generally blue to purplish-red. |
Hue is generally pink to red. |
| Tenderness |
Caused by palpation of the globe. |
Generally not caused by palpation of the globe. |
| Scleral edema |
Present. |
Absent. |
| Uveitis and peripheral ulcerative keratitis |
Present. |
Typically absent. |
Treatment of episcleritis associated with RA, in contrast to idiopathic episcleritis, usually requires oral NSAIDs, especially in recurrent cases. We have found Indocin (indomethacin, Merck) to be the most common oral NSAID used for both episcleritis and scleritis. We typically treat episcleritis in RA patients for four weeks with indomethacin 25mg q.i.d. and taper to t.i.d once we note improvement.
Treating scleritis is challenging and always requires oral and/or intravenous agents. NSAIDs, corticosteroids and immunosuppressive drugs are the mainstays of treatment for scleritis. Depending on the severity of both the ocular and systemic disease, treatment usually exceeds one to four months. We typically refer these patients to a corneal specialist.
RA is a debilitating disease, with less than 50% of working-age adults able to maintain employment 10 years after diagnosis.15 Fortunately, RA can be suppressed with early diagnosis and aggressive management. A diligent history and careful ocular examination will allow us to improve the ocular symptoms caused by RA.
We play an important role in the RA management team. Although our goal is to preserve our patients vision, we also have an obligation to improve their quality of life with proper care and treatment.
Drs. Black and Tyler are assistant professors and chiefs of their respective primary-care clinics at Nova Southeastern University College of Optometry. Dr. Kabat is an associate professor at Nova Southeastern and a contributing editor of Review of Optometry.
1. Ferucci ED, Templin DW, Lanier AP. Rheumatoid arthritis in American Indians and Alaska natives: a review of the literature. Semin Arthritis Rheum 2005 Feb;34(2):662-7.
2. Arthritis Foundation. Epidemiology. www.arthritis.org/conditions/diseasecenter/ra/ra_epidemiology.asp. Accessed October 21, 2005.
3. Harris Jr. Clinical features of rheumatoid arthritis. In: Kelleys Textbook of Rheumatology. Philadelphia: W.B. Saunders, 2001:967-96.
4. Matsumoto AK. Rheumatoid arthritis clinical presentation. www.hopkins-arthritis.org/rheumatoid/rheum_clin_pres.html. Accessed October 21, 2005.
5. The Merck Manual. Rheumatoid arthritis. www.merck.com/mrkshared/mmanual/section5/chapter50/50a.jsp. Accessed October 21, 2005.
6. Colglazier CL, Sutej PG. Laboratory testing in the rheumatic diseases: a practical review. South Med J 2005 Feb;98(2):185-91.
7. Ronnelid J, Wick MC, Lampa J, et al. Longitudinal analysis of citrullinated protein/peptide antibodies (anti-CP) during 5-year follow-up in early rheumatoid arthritis: anti-CP status predicts worse disease activity and greater radiological progression. Ann Rheum Dis 2005;64:1744-49.
8. Van Horn P. Patient handout: what you should know about rheumatoid arthritis. Female Patient 2004;29(1):104.
9. Maksymowych W, Russell AS. Antimalarials in rheumatology: efficacy and safety. Semin Arthritis Rheum 1987 Feb;16(3):206-21.
10. Patel SJ, Lundy DC. Ocular manifestations of autoimmune disease. Am Fam Physician 2002 Sep;66(6):991-8.
11. Jabs DA, Mudun A, Dunn JP, Marsh MJ. Episcleritis and scleritis: clinical features and treatment results. Am J Ophthalmol 2000 Oct;130(4):469-76.
12. Fuerst DJ, Tanzer DJ, Smith RE. Rheumatoid diseases. Int Ophthalmol Clin 1998 Fall;38(4):47-80.
13. Harper SL, Foster CS. The ocular manifestations of rheumatoid disease. Int Ophthalmol Clin 1998 Winter;38(1):1-19.
14. Foster CS. Recognizing the ocular manifestations of rheumatoid arthritis. Women Health Primary Care 1998;1(3):247-57.
15. Arthritis Foundation. Delivering on the promise in rheumatoid arthritis. www.arthritis.org/research/Research_Program/RA/default.asp. Accessed October 21, 2005.

