 |
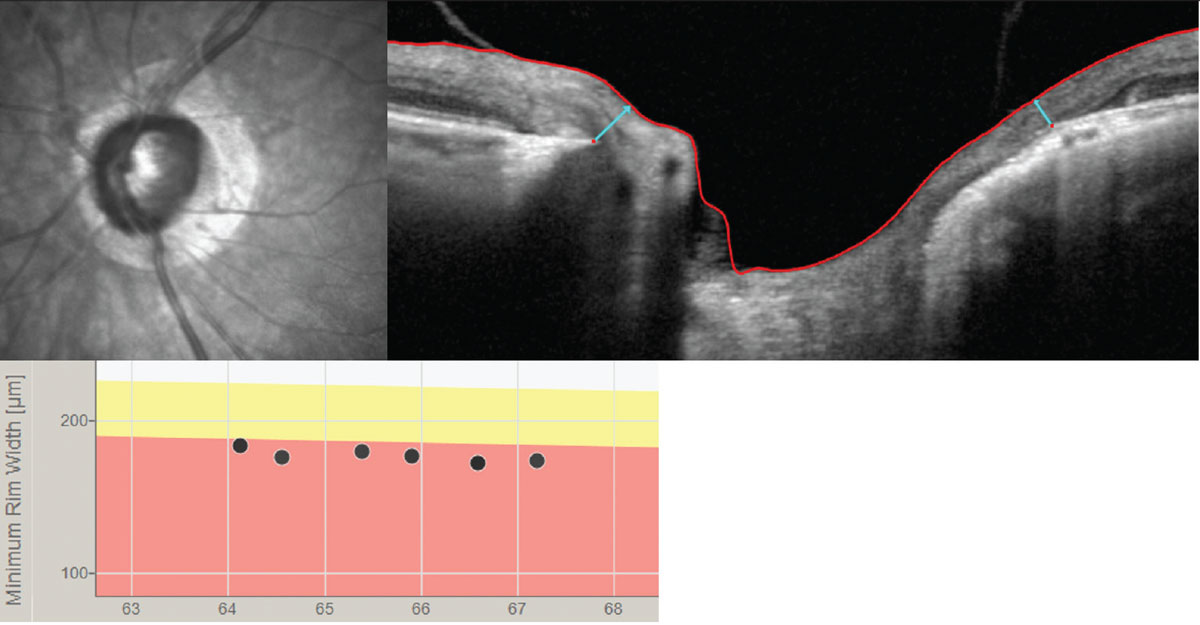
| A recent study has suggested there is likely value in looking beyond conventional neuroretinal parameters to landmarks such as laminar insertion points and Bruch’s membrane opening minimum rim width, as shown above. Photo: Andrew Rixon, OD. Click image to enlarge. |
Understanding structural changes in the optic nerve head (ONH), peripapillary retina and macula due to glaucoma is important for diagnosis and management. With rapid developments in OCT technology, image processing techniques that use artificial intelligence approaches are helping close this gap. A recent study published in JAMA Ophthalmology described the 3D structural differences in both connective and neural tissues of the ONH between different glaucoma stages using traditional and artificial intelligence-driven approaches. Notably, the majority of ONH structural differences occurred in the early glaucoma stage, followed by a plateau effect in the later stages. These changes were in both neural and connective tissues, with a stronger association seen in the superior and inferior quadrants.1
This cross-sectional, clinic-based study recruited 541 Chinese individuals and 112 Caucasian participants. All participants had their ONH imaged using spectral-domain OCT and had their visual field assessed by standard automated perimetry. Clinician-defined 3D structural parameters of the ONH and 3D structural landmarks identified by geometric deep learning that differentiated ONHs among four groups: no glaucoma, mild glaucoma (mean deviation [MD], ≥−6.00dB), moderate glaucoma (MD, −6.01dB to −12.00dB), and advanced glaucoma (MD, <−12.00dB).
Using a deep neural network, 3D ONH structural differences were found to be present in both neural and connective tissues. Specifically, a mean of 57.4% for no to mild glaucoma, 38.7% for mild to moderate glaucoma and 53.1 %, for moderate to advanced glaucoma of ONH landmarks that showed major structural differences were located in neural tissues with the remaining located in connective tissues.
“We observed that the decline in Bruch’s membrane opening minimum rim width slowed, whereas RNFL thickness decreased linearly as glaucoma severity increased,” the authors wrote in their paper. “This suggests that neural tissue changes in the early stage of glaucoma (normal to mild) are more pronounced around the optic disc (i.e., minimum rim width), in contrast to the later stages of glaucoma (mild to moderate and moderate to advanced), where such changes move to the periphery of the ONH (i.e., RNFL thickness).”
The team also found that most of the LC critical points gathered near the LC insertion zones. They were localized in the superior quadrant (normal-mild) and in both the superior and inferior quadrants (mild-moderate) but were more diffuse through the entire LC in late glaucoma stages (moderate-advanced).
“Assessing morphological changes of the glaucomatous lamina cribosa, especially in the region of the insertion zone, could be useful in monitoring disease progression,” the team also suggested.1
A commentary also published in JAMA Ophthalmology pointed out that “these conclusions are based on cross-sectional data, which pose significant limitations in informing us on longitudinal behavior.”2
“Imaging modalities with increased axial resolution may also allow segregation of neuronal and nonneuronal components in the rim and nerve fiber layer as these tissues remodel with age and glaucomatous loss,” the commentary added. “Adoption of artificial intelligence techniques will manage the increasingly large image arrays to provide clinically interpretable images and decision-making tools.”2
“Future longitudinal studies should seek to establish a connection between specific 3D ONH structural changes and fast visual field deterioration and aim to improve the early detection of patients with rapid visual field loss in routine clinical care,” the study authors concluded.1
1. Braeu FA, Chuangsuwanich T, Tun TA, et al. Three-dimensional structural phenotype of the optic nerve head as a function of glaucoma severity. JAMA Ophthalmol. August 17, 2023. [Epub ahead of print]. 2. Chauhan BC. Understanding the increasing role of optical coherence tomography in glaucoma diagnostics and disease progression. JAMA Ophthalmol. August 17, 2023. [Epub ahead of print]. |

