 |
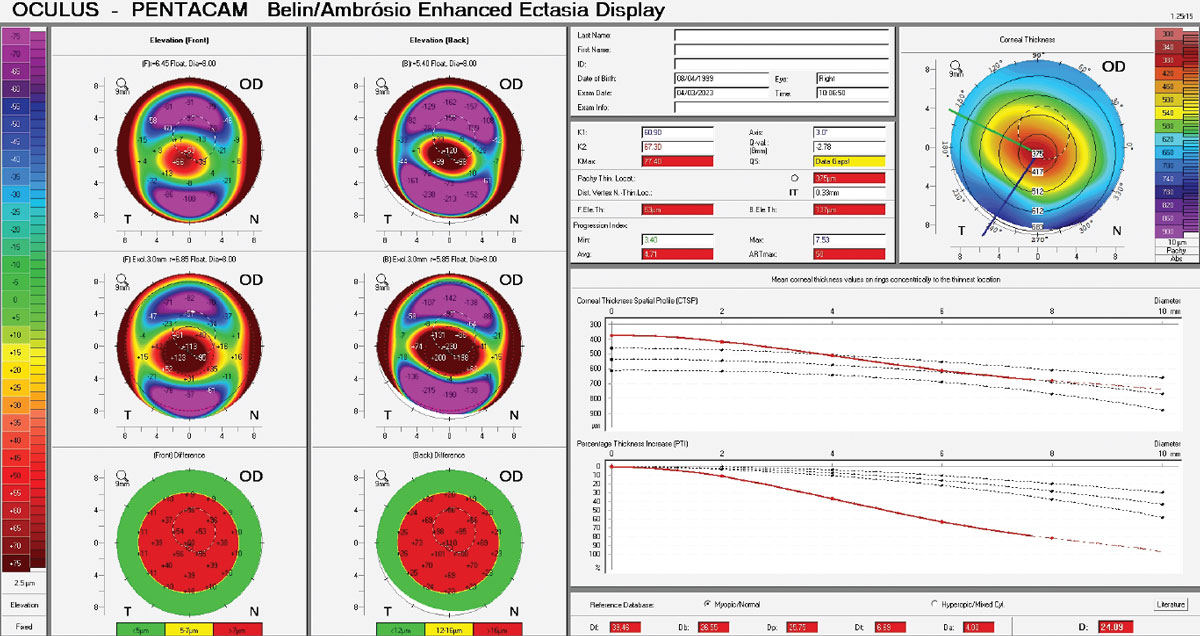
| The pachymetry progression index (PPI) calculates the change in corneal thickness from the thinnest point to the periphery. A rapid change in thickness indicates ectasia. This study found significant differences in PPI average and PPI max between patients at different stages of DR. Photo: Christine Sindt, OD. Click image to enlarge. |
Since individuals with diabetes are poor candidates for many forms of ocular surgery, it is necessary to be aware of the corneal changes induced by the condition to better plan any potential treatment strategies or refractive procedures. Also, comorbidities often cause poor refractive results and postoperative complications. Despite the widespread use of corneal topography and tomography, the possible effect of diabetes on corneal structural changes has not been well studied.
Researchers based in Iran recently compared corneal topographic indices between diabetic and non-diabetic elderly subjects while also considering their levels of diabetic retinopathy (DR) and diabetic control. The average and max pachymetric progression index (PPI) values were the most significantly different among unaffected subjects, those with diabetes and those with DR.
“The results of corneal topography indices in the elderly population aged 60 years and over with and without diabetes provide a suitable reference for comparison,” the research team noted in their paper.
Using random cluster sampling, a total of 1,105 participants from Tehran—including 429 diabetes patients (38.5% male) and 676 non-diabetic (38.8% male) subjects—participated in the study. The diabetic group had HbA1c levels ≥6.4% with no other systemic problems. Of the diabetic patients, 85.3% did not have DR while 11.0%, 1.4%, 1.2% and 1.2% had mild non-proliferative DR (NPDR), moderate NPDR, severe NPDR and PDR, respectively.
Only average PPI and max PPI values were higher in those with diabetes vs. unaffected subjects. “Tomography-derived pachymetric indices such as PPI values are better for the differential diagnosis of normal from abnormal corneas compared with single-point corneal thickness measurements,” the researchers proposed in their article. They were aware that the study’s cross-sectional design made it impossible to evaluate the causal relationship between diabetes and corneal topography indices. Also, they did not evaluate the corneal endothelium, which they recommend future studies explore.
“Several corneal topographic parameters change following hyperglycemia and the presence of DR,” the study concluded. “Special attention should be paid to these patients for different treatment strategies.”
Hashemi A, Khabazkhoob M, Narooei F, et al. Corneal topographic indices of scheimpflug camera in type 2 diabetic and non-diabetic elderly populations. BMC Ophthalmol. 2023;23(1):427. |

