 |
|
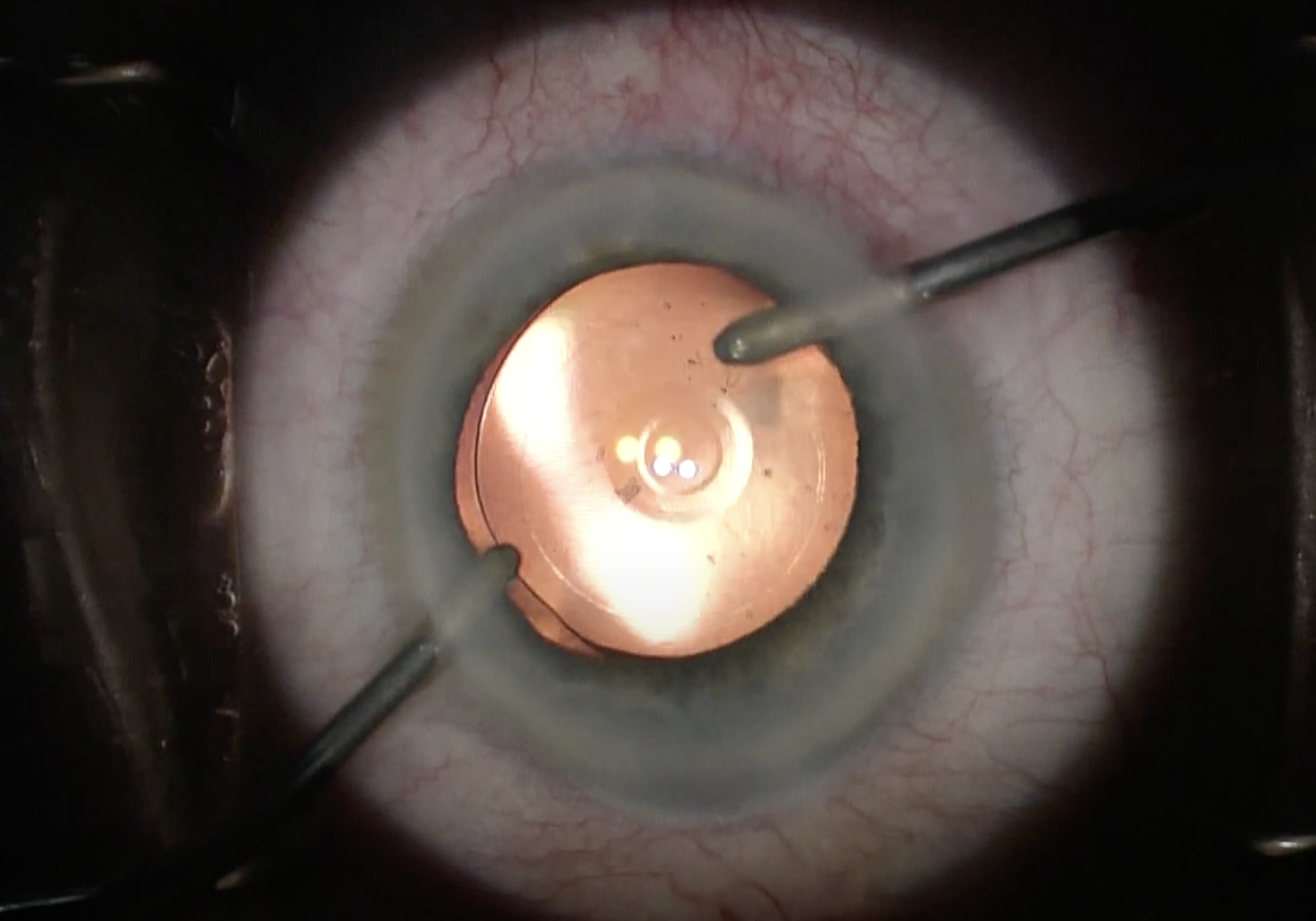
Sex differences have been observed in other aspects of eye care, including accessibility, cataract surgery timing, retinal detachment repair and subjective visual impairment, adding to the list the observed greater likelihood of visual improvement after IOL exchange. Photo: Alcon. Click image to enlarge. |
Cataract surgery is generally quite safe and successful, but a small number of patients may need to undergo a second procedure for intraocular lens (IOL) exchange. As data on lens replacement surgeries is somewhat lacking, researchers recently examined data collected from the Intelligent Research in Sight (IRIS) registry from such patients to look for patterns, publishing their findings in Ophthalmology.
The retrospective analysis specifically assessed risk factors leading to worse visual acuity (VA) outcomes after exchange as well as the most common postsurgical complications. Patients who underwent the procedure were included over six consecutive years, totaling 46,063 procedures from 41,925 unique patients. VA improved on average from baseline to one year postoperatively from 20/70 to 20/40. Of eyes with VA recorded at baseline and one-year post-op, 60.5% achieved VA of 20/40 or better at one year; only 9% had VA worse than 20/200. VA worse than this at one year was found linked to greater age, higher baseline VA, Black, Hispanic or Asian ethnicity, Medicaid over private insurance, smoking, and concurrent anterior or posterior vitrectomy over no vitrectomy.
Conversely, female sex was found to be associated with higher likelihood of visual improvement with vision of 20/40 or better at one year. The most common complications at this one-year mark were epiretinal membrane (10.9%), mechanical lens complication (9.4%) and dislocation of replacement lens (7.1%). Other, less common complications occurred, including retinal detachment (6.7%), glaucoma (6.5%) and chronic corneal edema or decomposition (4.6%).
In their discussion, the study authors attribute the association of older age to poorer vision to be due to ocular comorbidities often seen with greater prevalence in that population. As well, increased age has been linked to worse postoperative outcomes with both cataract and vitreoretinal surgery, even without coexistent ocular diseases. Similarly, concurrent anterior or posterior vitrectomy are thought to contribute to worse outcomes also because fewer comorbidities were seen in the group only receiving bag-to-bag exchange. The ethnic disparities observed are thought to potentially be due to differences in IOL exchange indications or severity of ocular comorbidities as contributing factors.
Like previous literature, this study’s IOL dislocation rate was comparable, with previous reports citing 2.1% to 7.7%. Other complications were also similar in previous reports, with instances of retinal detachment ranging from 1% to 21% and glaucoma observed in 7.1% to 17.3% or cases.
One thing the authors particularly pay attention to is the rate of IOL exchange increasing over the six years observed in this study. They conclude that “the significant rise in the rate of IOL exchange over time is a trend that warrants attention and further research into both prevention and management. This also points to the importance of improving the education and skills transfer training of anterior and posterior segment surgeons who will increasingly need to perform this procedure in the future.”
Son HS, Chang DF, Li C, et al. Visual acuity outcomes and complications after intraocular lens exchange: an IRIS Registry analysis. Ophthalmology. October 17, 2023. [Epub ahead of print]. |

