 |
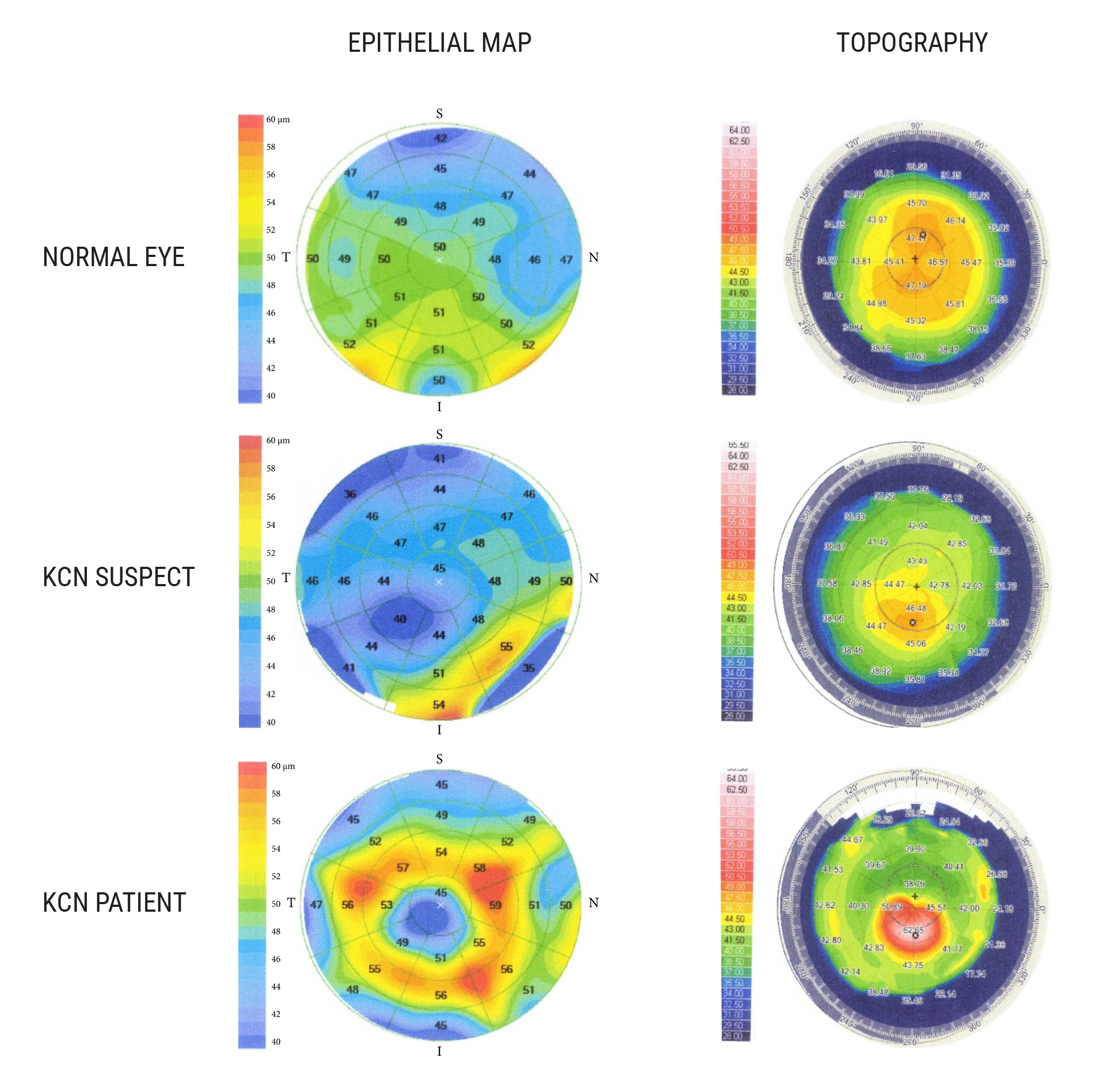
| To strengthen the ability of OCT-derived data to detect subclinical keratoconus, researchers suggest that coupling epithelial thickness profiles with corneal tomography may prove beneficial in future studies. Photo: Salman A, et al. J Ophthalmol. 2023;6677932. Click image to enlarge. |
Better diagnostic tools continue to raise our estimates of the prevalence of keratoconus (KC), as devices get increasing sophisticated about recognizing the telltale signs. Consequently, many optometry practices are devoting more time to the detection and management of this progressive disease typically characterized by thinning of the stroma, most prominently in the 5mm zone. OCT-derived data, such as total corneal thickness (CT) and epithelial thickness (ET), are often used to help identify the condition; however, the diagnostic accuracy of these measurements remains unclear. A recent study put the sensitivity of these parameters to the test and landed on two primary conclusions: while CT and ET could reliably differentiate between KC and normal eyes, it was range of minimum-to-maximum (min-max) epithelial thickness that, to a lesser extent, showed the most robust ability to detect suspect disease.
The researchers divided a total of 144 eyes between three groups: normal (n=65), suspect KC (n=43) and KC (n=36). CT and ET in the central (0mm to 2mm) and paracentral (2mm to 5mm) zones were obtained using a Zeiss Cirrus 5000 HD-OCT.
The data revealed that neither ET nor CT variables were strong enough on their own to differentiate between suspect KC and normal eyes, although the two parameters showing the highest diagnostic power were min-max ET and central CT. The researchers noted in their paper for Journal of Ophthalmology that these “findings are consistent with a previously reported study, where the authors found that central CT was the parameter with the highest ability to differentiate between subclinical KC and normal eyes.”
On the other hand, when differentiating between clinical KC and normal eyes, ET and CT both performed with a high level of certainty. Analysis revealed excellent predictive ability to detect keratoconus for the following ET variables: minimum ET, min-max ET and superonasal-inferotemporal ET . For total corneal thickness parameters, min-max CT was the only one to show an excellent ability to discriminate between KC and normal eyes.
“Coupling ET profiles with corneal tomography may further aid in screening for KC and may be useful in the clinical setting,” the researchers proposed based on their findings. “ET data may allow for an earlier diagnosis of KC, as epithelial changes may precede any changes produced on the front surface of the cornea.”
Because this study found that the use of a single parameter to diagnose subclinical KC was insufficient, the researchers conclude that future research will use a “combination of OCT-derived data with posterior corneal surface and wavefront data to improve automatic recognition of early KC.”
Salman A, Mazzotta C, Kailani O, et al. diagnostic accuracy of corneal and epithelial thickness map parameters to detect keratoconus and suspect keratoconus. J Ophthalmol. 2023;6677932. |

