Age-related macular degeneration (AMD) is a retinal disease that affects millions of people globally. An estimated 288 million people are predicted to have AMD by 2040.1 With a worldwide prevalence of 8.7%, it is one of the leading causes of irreversible blindness and vision impairment.
AMD primarily affects people later in life, and patients 55 and older should be screened for the condition through a dilated fundus evaluation and risk assessment profile.2 Risk factors for developing AMD include a positive family history especially in first-degree relatives, cigarette smoking and Caucasian race. Additionally, factors such as female sex, increased exposure to sunlight, cardiovascular disease, diet and light-colored irises may be potential risk factors.1-4
In AMD, there is characteristic drusen formation and pigmentary alteration in the macular region. Patients must have at least one druse that is intermediate in size (greater than 63µm and less than 125µm) to be diagnosed with early AMD.4,5 As the condition progresses, there is loss of the photoreceptor layer and disruption of the retinal pigment epithelium (RPE), which may be due to oxidative damage, leading to geographic atrophy (GA).2,3 This is the dry form of late or advanced AMD. In some cases, there is growth of new and abnormal blood vessels stimulated by vascular endothelial growth factor (VEGF).4 This is known as wet or neovascular AMD.
 |
|
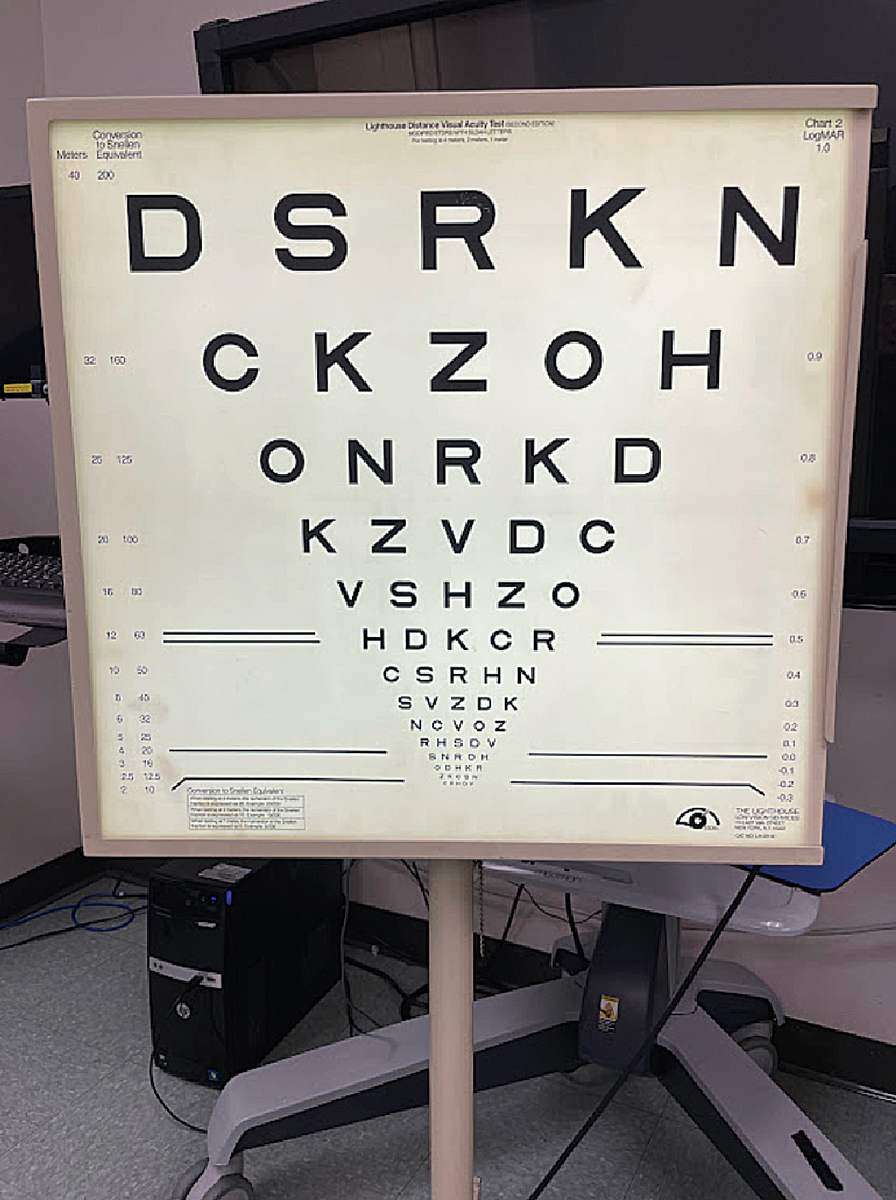
Fig. 1. The ETDRS chart can be placed at 4m, 2m or 1m. Click image to enlarge. |
Dry vs. Wet
Approximately 90% of patients with AMD have the dry form.4 For treatment of dry AMD, the Age-Related Eye Disease Study (AREDS) showed that a formulation of high-dose vitamins C and E, beta carotene and zinc helped reduce the risk of progression to advanced stages, defined as either the development of choroidal neovascularization or central GA. The use of AREDS vitamins was shown to be beneficial for those with either extensive intermediate drusen, one or more large drusen, noncentral GA in one or both eyes or advanced AMD in one eye.2
AREDS2, a follow-up study looking at the benefits of changing the treatment formulation, found no benefit from the addition of omega-3 fatty acids, lutein or zeaxanthin. However, the study suggested that in patients with a history of smoking, there is a potential increased risk of lung cancer when using formulations that include beta carotene. The AREDS2 study concluded that lutein and zeaxanthin could be used as substitutes.5
Other management strategies include intake of leafy green vegetables, protection against UV exposure and discontinuation of smoking.4 Additionally, studies are looking to see if medications, such as the complement inhibitor eculizumab, or gene therapy can be employed to treat GA.6
While less common than the dry form, wet AMD is responsible for 90% of cases with severe vision loss, which is defined as loss of six or more lines of distance acuity.7 Medical treatment options are currently only available for wet AMD and include laser photocoagulation, photodynamic therapy (PDT) and anti-VEGF injections.2,7,8 Laser photocoagulation targets melanin in the RPE to destroy neovascularization. However, it leaves behind an absolute scotoma due to the damage to the overlying retina and RPE and is becoming less commonly used in the treatment of exudative AMD.8 PDT was developed to minimize this damage and selectively target the neovascularization. It has been shown to prevent loss in approximately two-thirds of treated patients, though moderate vision loss still occurs despite treatment.7 Anti-VEGF intravitreal injections such as bevacizumab, ranibizumab or aflibercept can be administered to control neovascularization and regress vessel growth, with current studies looking at best follow-up practices and combination therapies for this first-line treatment.4,9
As many patients go on to develop some form of vision loss, even in the presence or as a side effect of treatment, it is important to understand how this vision loss may present clinically. With both forms of AMD, there can be a reduction in best-corrected visual acuity (BCVA), loss of contrast sensitivity, development of central and paracentral scotomas, decrease in stereopsis and delay in dark adaptation. Patients also develop an inability to perform activities of daily living (ADL). They may present with a multitude of complaints such as poor vision, difficulty driving, reading, recognizing faces and glare sensitivity. These patients should be evaluated by eyecare providers to determine if tools and strategies beyond traditional glasses and contact lenses can be used to improve visual function and quality of life (QoL).
 |
|
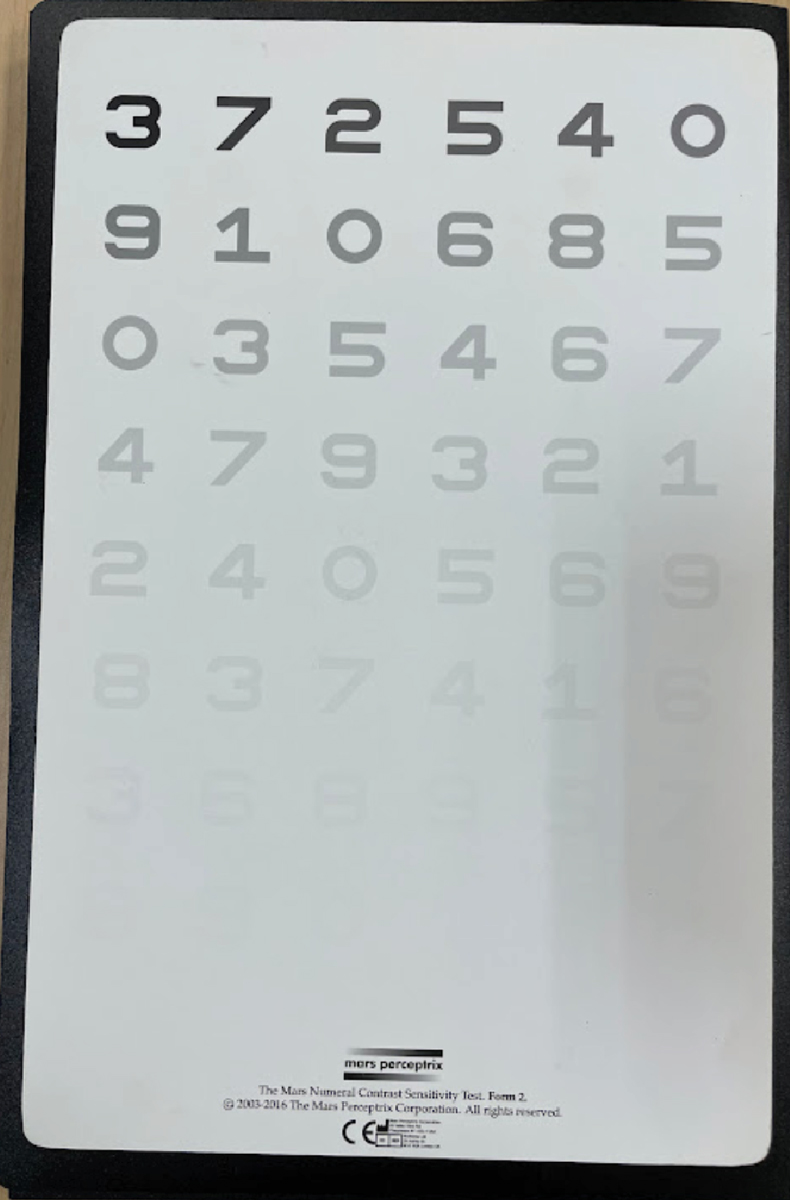
Fig. 2. A Mars contrast set comes with three cards, available in both letters and numbers. Click image to enlarge. |
Visual Acuity Changes
This may be noticed initially by the patient as they start experiencing difficulty seeing fine print and details. They may report things like blurry vision at all distances and difficulty reading street signs, menus and medication labels. In patients with AMD, visual acuity is what determines legal blindness, defined as BCVA of 20/200 or worse in the better-seeing eye or a visual field of no more than 20° in its widest meridian in the eye with the larger field.10 The visual field qualification is unlikely in patients with macular degeneration alone, as the peripheral visual field is spared. However, if patients have other conditions that affect the peripheral field such as glaucoma, they may qualify in that manner.
Resolution visual acuity can be measured using traditional vision charts such as the Snellen chart and the Early Treatment Diabetic Retinopathy Study (ETDRS) chart, with the type of chart (e.g., paper, projector, digital, etc.) affecting a patient’s results (Figure 1). While the Snellen chart is widely used in the clinical setting, there are several flaws to its design that affect measurement of visual acuity in patients with visual impairment. For instance, there is only one line (20/200) between 20/100 and 20/400, which makes measuring acuity at these levels difficult.6
Patients with visual impairment typically perform better with less variable results using an ETDRS chart, especially in cases of advanced disease with vision worse than 20/200. The ETDRS chart allows for accurate measurement of low levels of acuity because it has more lines and the working distance can be adjusted from 4m in cases of even poorer acuity to 2m or even 1m. The consistency of the type on the chart also makes it easier to read. Additionally, the ETDRS chart is used exclusively in clinical studies while case reports tend to be published using Snellen notation.11
While measuring visual acuity is a key part of the examination, this component alone does not paint a complete picture of the visual function, or loss thereof, in patients with AMD. Visual acuity on high-contrast vision charts may remain intact while other aspects of visual function such as contrast sensitivity degrade over time. In addition, reading isolated optotypes one by one on a visual acuity chart may still be achievable while advancing GA continues to snuff out vision and create larger paracentral scotomas.
 |
|
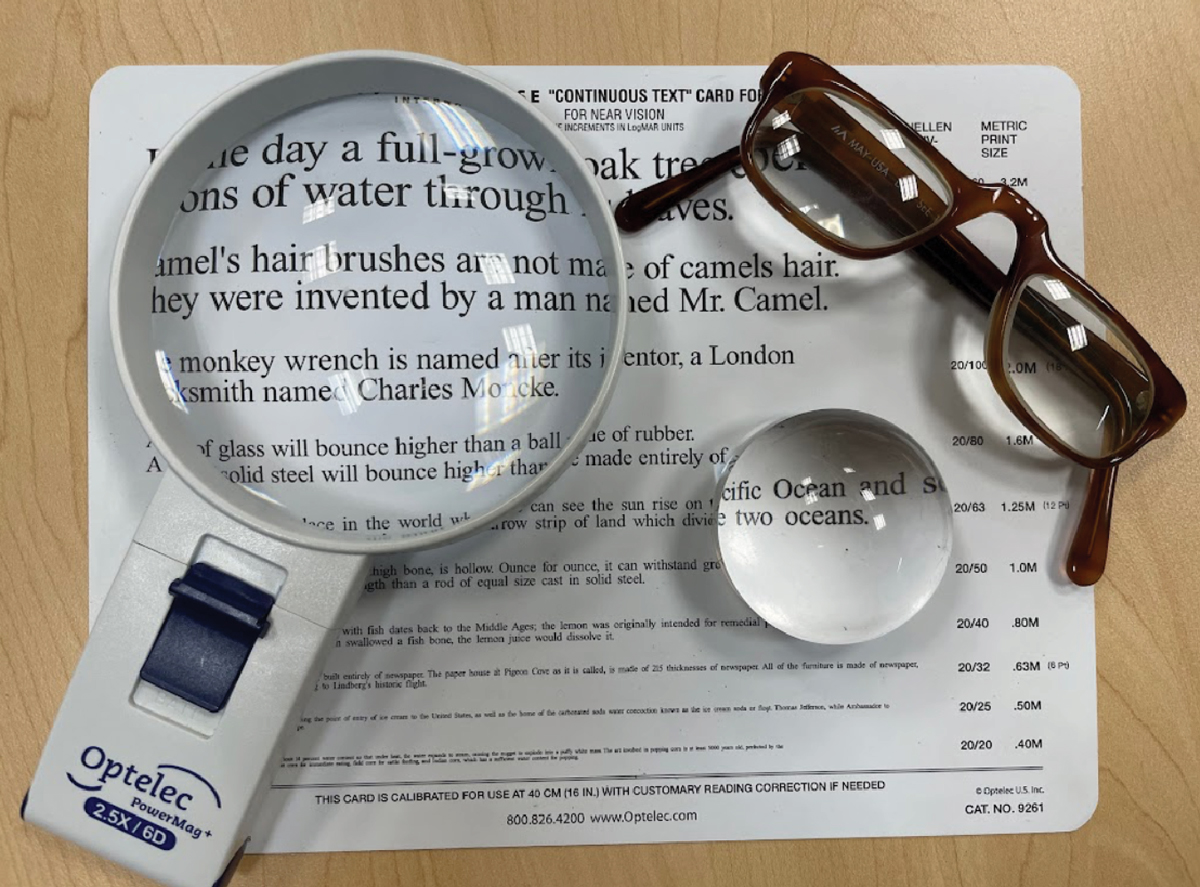
Fig. 3. A monocular handheld telescope (left) and a binocular telescope in a frame. Click image to enlarge. |
Contrast Sensitivity Concerns
This plays a large role in many ADLs and can be more indicative of functional difficulties than changes in acuity.12,13 Patients with AMD require higher luminance and contrast for letter recognition, which affects general visual function. They may report difficulty seeing in low-light environments, such as in subway stations and restaurants or in poor weather conditions. They may also have increased sensitivity to glare and difficulty reading low-contrast media such as newspapers. Words like “foggy” or “hazy” are commonly used to describe their vision. Additionally, contrast sensitivity affects a patient’s reading ability, with reduced contrast leading to reduced reading ability and speed.13
Clinically, there are many ways to determine contrast sensitivity. It is commonly measured with either a Mars or Pelli-Robson chart based on the patient’s acuity level (Figure 2). The Mars chart has been shown to produce reliable and repeatable results in patients with BCVA of 20/250. It is smaller than the Pelli-Robson and is printed on a hard material as opposed to cardboard, making it a more convenient, portable and accessible tool in clinical settings.14 Digital visual acuity charts can often measure contrast in addition to standard high-contrast acuity, though the functionality differs depending on the system.
Contrast loss is categorized as moderate, severe or profound and can be confounded by other factors such as cataracts and dry eye, which are often comorbidities in these patients. Contrast testing should be considered in all patients with AMD as an additional method of monitoring change and visual impact of the condition.
The Overlap: AMD and GABy Kathryn Deliso, OD A risk assessment profile is an essential element of the case history when evaluating patients older than 55 or those with clinical features or risk factors of AMD and GA. Studies show that genetics likely play a role in almost three out of every four cases of AMD; this association is even stronger in GA.1 There are two genes most closely related to the development of AMD: complement factor H Y4402H polymorphism, chromosome 1q32, and the ARMS2/HTRA1 gene, chromosome 10q26.13.1,2 The risk is additive, so a patient with both genes is at the greatest risk of AMD.1 Those with high-risk genes are not only more susceptible to developing AMD but are also at elevated risk of progressing to legal blindness.1,2 Address a patient’s risk profile at the initial visit, prioritizing modifiable risk factors to maximize the impact of early intervention and reduce the overall risk of significant vision loss secondary to AMD. One of the greatest impact factors for early risk intervention is smoking, as smokers have a two to three times greater risk of developing AMD.3 In addition, smokers develop AMD at a younger age and have a higher risk of disease progression.3 Fortunately, smoking cessation results in a reduction of risk commensurate with the duration of abstinence from tobacco, with studies reporting that former smokers are at only slightly higher risk than people who have never smoked.4,5 Macular EvaluationIn cases of central binocular vision impairment where the fovea becomes nonfunctional more so in one eye than the other, the neuroplastic visual system can adapt by creating a new pseudo-fovea, termed the preferred retinal locus. The function of the peripheral retina to fixate a target due to a central scotoma has been investigated extensively and has since become an important part of the rehabilitation plan for patients with retinal disease and foveal sparing.6 Microperimetry, or scanning laser ophthalmoscopy, measures light sensitivity of the retina by projecting Goldmann III stimuli over different retinal locations. Retinal images are then processed by an eye tracker to calculate and compensate for fixation losses, allowing vision rehabilitation specialists to objectively assess fixation stability. Patients with bilateral central vision loss from GA and those with the potential to eccentrically view may benefit from this technology, as it uses biofeedback signals as auditory confirmation of the patient accurately accessing the appropriate eccentric viewing posture. Vision RehabilitationUnlike neovascular AMD, GA progresses slowly and spares the foveal center until late in the course of the disease. These patients might present with seemingly preserved central acuity and functional complaints disproportionate to their best-corrected acuity. A low vision evaluation for patients with GA includes assessment of scotomas, reading rate and fluency, as parafoveal scotomas impair visual performance by limiting the size of the seeing central region so that only a portion of a word or a facial feature can fit in the seeing area. Acuity and reading rate may be critically dependent on character size for individuals with GA.7,8 Reading rate of continuous text with calculations of the equivalent power a patient might need to resolve text, spot-read text or continuously read text should be conducted in cases of GA. Research has shown that when the foveal center is involved, the size of the atrophic area is a critical determinant of reading rate. This association suggests a correlation between the patient’s functional impairment and the size of the atrophic retina.7,8 Dr. Deliso is an associate professor of optometry and chief of vision rehabilitation at the MCPHS School of Optometry in Worcester, MA.
|
Central Scotomas
Many patients with AMD develop central scotomas due to macular atrophy or as a side effect of laser photocoagulation, both of which affect visual acuity and contrast sensitivity negatively. Scotomas due to pathology may also continue to change as the condition progresses. Patients may complain of difficulty keeping their place while reading and recognizing faces. They may report areas of distortion or objects that “appear out of nowhere” rather than dark spots in their vision.15
Traditional visual field testing is difficult for patients with poor fixation, such as in AMD, but microperimetry, also referred to as fundus perimetry, can be used to map these central scotomas and track their progression over time. Microperimetry uses tracking software to account for the location and stability of fixation, which allows for more accurate and real-time documentation of retinal sensitivity than traditional methods. These results can also be overlaid on a fundus photograph.16 The Amsler grid is another option that is widely accessible and doubles as an educational device and home monitoring aid for the patient to check for any changes in their vision between appointments.
In a healthy eye, the fovea has the highest density of cone photoreceptors, allowing for maximum visual acuity. However, because of central scotomas, patients with AMD may develop eccentric viewing, where they fixate using non-foveal points. As the peripheral retina is not as efficient in word recognition and processing, these patients experience reduced visual span and temporal processing.17,18 They have more difficulty reading and slower reading speeds than patients with reduced central acuity alone.15,17 Studies have shown that reading is the primary concern when patients with AMD seek further treatment, with over 85% reporting difficulty in this region.19
Patients with macular degeneration can also have poor stereopsis and difficulty with binocular function as they lose central vision due to the brain’s inability to fuse dissimilar images. While there are still monocular cues, disparate images seen by both eyes are required for depth perception. One study showed a loss of stereopsis due to reduced acuity and contrast sensitivity where age-matched patients with normal acuity and contrast sensitivity did not experience any loss.19 Another found that patients with AMD and stereopsis had higher overall functional visual abilities with better reading abilities, visual motor skills and mobility skills than those who did not. There was no correlation with BCVA between the two groups.20
Loss of stereopsis can also present as difficulty with mobility, such as navigating curbs and steps and reaching for objects, and general clumsiness including knocking over glasses or spilling when pouring. It can affect a patient’s ability to drive, even if acuity and fields remain intact in one eye. There are many methods of measuring stereopsis during a clinical exam, one example being traditional stereoacuity test booklets. Follow-up with questions regarding the patient’s visual function for further evaluation and management.
 |
|
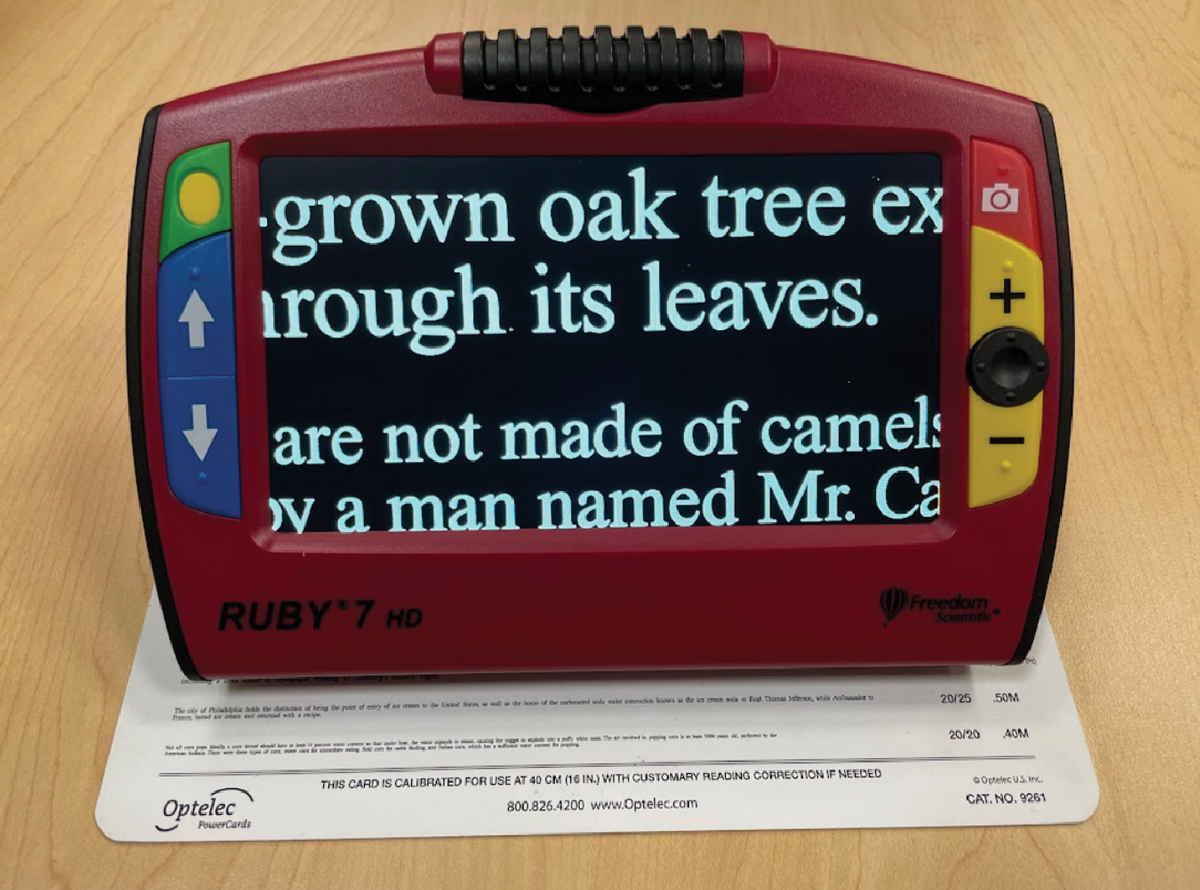
Fig. 4. An illuminated handheld magnifier (left), a dome magnifier—a type of stand magnifier (middle)—and a pair of prism half eye glasses. Click image to enlarge. |
Management and Rehabilitation
AMD can affect the visual system in many ways, and the impairment is usually permanent. A study performed on vision-related QoL showed the importance of high contrast acuity and contrast sensitivity and how vision loss secondary to AMD negatively affects both visual function and the socioemotional status of patients. Tasks such as reading, driving and facial recognition are all critical to vision-related QoL and drive patients to seek further services.19,21
Additionally, vision-related QoL is directly related to the severity of vision loss.7 Rehabilitation is important to keep in mind in the comprehensive management of patients with AMD. Patients with even a small amount of visual impairment may find it difficult to perform ADLs and could benefit from low vision services. This also holds true when the impairment is only monocular. Early referral is critical, especially as the condition is progressive. Low vision rehabilitation refers not only to optical management but also to training, counseling and other interventions through collaboration with rehabilitation specialists.
Low vision management of patients with AMD starts with an expanded functional history. Providers need to understand the patient’s specific goals and use this information in conjunction with exam findings to offer the most appropriate recommendations. Factors to consider include working distance for the task, portability of the device and patient ability to physically manipulate the device. Management beyond traditional glasses and contact lenses includes the use of devices for distance and near, contrast enhancement and glare reduction. Non-optical aids, orientation and mobility training and traditional vision therapy techniques can also be employed. Management for patients with AMD should be personalized and aim to improve QoL and independence.
The exam should start with an accurate refraction to determine the patient’s BCVA. One study found that 11% of new low vision patients showed improvement of two lines of acuity or more through refraction alone.22 A trial frame refraction rather than a traditional phoropter refraction is recommended for these patients to allow for eccentric viewing as needed. For near add determination, these patients may require a higher add, which requires shortening of the working distance. This should be prescribed as a pair of separate reading glasses, as a high add in a multifocal lens can increase the risk for falls.
For further distance enhancement beyond refractive correction, telescopes may be used (Figure 3). Telescopes can be monocular or binocular, handheld or spectacle-mounted. They are used for spotting distant objects such as street signs, not for ambulation. Training is needed to teach patients proper techniques to best work the device. Spectacle-mounted telescopes may be prescribed for driving in some states with appropriate patient selection, training and rehabilitation.
For near enhancement, options include high-powered adds, handheld magnifiers, stand magnifiers and electronic magnification (Figures 4 and 5). While magnifiers can be purchased at many retailers and stores, patients should undergo an evaluation with an eyecare provider to find the magnifier that is best suited for their visual needs. Personal electronic devices such as smartphones or computers have built-in accessibility features, and additional applications and programs can be downloaded to magnify items on the screen. Cameras in smartphones and electronic magnifiers can also magnify objects in real life. Additionally, some applications may take advantage of the microphone and speaker to read text on the screen and respond to verbal cues. Training may be required to learn the techniques needed to use these devices effectively.
Contrast enhancement can be achieved through changes in illumination, the use of colored filters or tints and electronic contrast enhancement. Bright and even illumination is important. Patients may want to consider installing additional lights in typically darker rooms of their house, such as the hallway or closet. Stick-on lights can be placed under shelves and cabinets. Fitover-style sunglasses can be used to alleviate glare reduction, both indoors and outdoors. These sunglasses are designed to go over glasses and block excess glare. Low vision electronic magnifiers typically have multiple different contrast modes, such as enhanced negative contrast where text is displayed as white on a black background, which may be beneficial to the patient.
 |
|
Fig. 5. An example of a portable electronic magnifier displaying enhanced negative contrast. Click image to enlarge. |
Additionally, personal electronic devices such as smartphones and computers can be adjusted for brightness levels and different contrast settings. For example, a smartphone can be set so that text will display as white on a black background. This can improve both visual ability and comfort. It has been suggested that patients with low vision also read faster using reverse-polarity text, which creates a darker background than the text, likely due to an increase in depth of focus.18
Non-optical resources and management strategies should be considered as well, as there are many devices designed for patients with visual impairment to help them complete specific tasks that may otherwise be difficult. For example, patients with contrast loss may benefit from a bold-tipped pen for writing. When the service is available, they can request materials in large print, including medication labels, newspapers and novels. Tools such as liquid level indicators and large-print wristwatches are also options.
Mobility training by a specialist may be beneficial to acquire techniques for safe and independent navigation, as patients may experience difficulty ambulating with their reduced vision due to decreased acuity, contrast and stereopsis and the presence of scotomas. This training does not necessarily refer to a mobility cane or guide dog, as these tools are selected by rehabilitation therapists based on the patient’s specific requirements.
Referral to occupational therapy may also be beneficial, as patients can work one-on-one with a therapist to enhance performance in areas such as reading, grooming, meal preparation, eccentric viewing techniques and low vision device use.23
Even with appropriate magnification, patients with central scotomas still have difficulty reading.17 Traditional vision therapy techniques supplemented with home therapy activities can be used to improve visual performance in these patients by enhancing saccades and pursuits.18,24
In addition to visual changes, there can be a profound psychosocial impact on patients as they experience progressive vision loss. Vision plays a significant role in the way we interact with the world, and loss thereof can be discouraging and isolating. Patients often express anger, frustration, sadness and distress that their eyes do not work as they once did. The Patient Health Questionnaire-2 can be used to screen for depression. These patients can benefit from services such as talk therapy, which is available in person, over the phone or through video conferencing, making it more accessible to everyone.25
Patients with vision loss, especially central as in AMD, can experience visual phenomena such as photopsia or formed images that are not physically present. In the AREDS2 study, nearly 90% of participants reported this side effect at least once during the 10 years of follow-up.5 This occurrence, Charles Bonnet syndrome, can be an alarming experience for patients who are not properly educated on the condition. They should be reassured that these experiences are common and on their own, do not indicate neuropsychiatric disorders.26 However, further workup may be needed to clarify the etiology, as visual phenomena can also be a side effect of medications or other conditions.
Takeaways
AMD is a condition that affects a substantial number of patients globally and causes multiple functional vision problems. There is a combination of both modifiable and nonmodifiable risk factors, and treatment is only available for certain forms of the disease. Many of these patients experience some form of vision loss and must be monitored carefully and made aware of resources such as low vision rehabilitation. Candidates should be referred for these services at an early stage and given tools to help them continue performing ADLs independently
Dr. Lin is a graduate of the University of California Berkeley School of Optometry. She completed a residency in low vision rehabilitation at SUNY College of Optometry, where she currently works as an assistant clinical professor. She has no financial interests to disclose.
1. Wong WL, Su X, Li X, et al. Global prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: a systematic review and meta-analysis. Lancet Glob Health. 2014;2(2):e106-16. 2. Fine SL, Berger JW, Maquire MG, Ho AC. Age-related macular degeneration. N Engl J Med. 2000;342(7):483-92. 3. Beatty S, Koh H, Phil M, et al. The role of oxidative stress in the pathogenesis of age-related macular degeneration. Surv Ophthalmol. 2000;45(2):115-34. 4. Bowling B. Age-related macular degeneration. Kanski’s Clinical Ophthalmology. WB Saunders. 2015;8:598. 5. Age-Related Eye Disease Study 2 Research Group. Lutein + zeaxanthin and omega-3 fatty acids for age-related macular degeneration: the Age-Related Eye Disease Study 2 (AREDS2) randomized clinical trial. JAMA. 2013;309(19):2005-15. 6. Yehoshua Z, de Amorim Garcia Filho CA, Nunes RP, et al. Systemic complement inhibition with eculizumab for geographic atrophy in age-related macular degeneration: the COMPLETE study. Ophthalmology. 2014;121(3):693-701. 7. Ambrecht A, Aspinall PA, Dhillon B. A prospective study of visual function and quality of life following PDT in patients with wet age related macular degeneration. Br J Ophthalmol. 2004;88(10):1270-3. 8. Bylsma GW, Guymer RH. Treatment of age-related macular degeneration. Clin Exp Optom. 2005;88(5):322-34. 9. ANCHOR Study Group. Ranibizumab versus verteporfin photodynamic therapy for neovascular age-related macular degeneration: two-year results of the ANCHOR study. Ophthalmology. 2009;116(1):57-65. 10. Disability Evaluation Under Social Security, XVI U.S.C 2.0 et ceq. 11. Falkenstein IA, Cochran DE, Azen SP, et al. Comparison of visual acuity in macular degeneration patients measured with snellen and early treatment diabetic retinopathy study charts. Ophthalmology. 2008;115(2):319-23. 12. Bellmann C, Unnebrink K, Rubin GS, et al. Visual acuity and contrast sensitivity in patients with neovascular age-related macular degeneration. Graefes Arch Clin Exp Ophthalmol. 2003;241:968-74. 13. Rubin GS, Bandeen-Roche K, Huang GH, et al. The association of multiple visual impairments with self-reported visual disability: SEE project. Invest Ophthalmol Vis Sci. 2001;42(1):64-72. 14. Dougherty BE, Flom RE, Bullimore MA. An evaluation of the Mars Letter Contrast Sensitivity Test. Optom Vis Sci. 2005;82(11):970-5. 15. Schuchard RA. Preferred retinal loci and macular scotoma characteristics in patients with age-related macular degeneration. Can J Ophthalmol. 2005;40(3):303-12. 16. Midena E, Pilotto E. Microperimetry in age: related macular degeneration. Eye (Lond). 2017;31(7):985-94. 17. Cheong AMY, Legge GE, Lawrence MG, et al. Relationship between visual span and reading performance in age-related macular degeneration. Vision Res. 2008;48(4):577-88. 18. Chung STL. Reading in the presence of macular disease: a mini-review. Ophthalmic Physiol Opt. 2020;40(2):171-86. 19. Schneck ME, Haegerstrom-Portnoy G, Lott LA, Brabyn JA. Ocular contributions to age-related loss in coarse stereopsis. Optom Vis Sci. 2000;77(10):531-6. 20. Cao KY, Markowitz SN. Residual stereopsis in age-related macular degeneration patients and its impact on vision-related abilities: a pilot study. J Optom. 2014;7(2):100-5. 21. Roh M, Selivanova A, Shin HJ, et al. Visual acuity and contrast sensitivity are two important factors affecting vision-related quality of life in advanced age-related macular degeneration. PLoS One. 2018;13(5):e0196481. 22. Sunness JS, El Annan J. Improvement of visual acuity by refraction in a low-vision population. Ophthalmology. 2010;117(7):1442-6. 23. Smallfield S, Kaldenberg J. Occupational therapy interventions for older adults with low vision. Am J Occup Ther. 2020;74(2):7402390010p1-7402390010p5. 24. Marinoff R. Using vision therapy to maximize visual efficiency for low vision patients with central scotoma. Optom Vis Perfor. 2016;4(1):43-50. 25. Holloway EE, Sturrock BA, Lamoureux EL, et al. Depression screening among older adults attending low-vision rehabilitation and eye-care services: characteristics of those who screen positive and client acceptability of screening. Australas J Ageing. 2015;34(4):229-34. 26. Age-Related Eye Disease Study 2 Research Group. Associations between age-related eye diseases and Charles Bonnet Syndrome in participants of the Age-Related Eye Disease Study 2: Report Number 26. Ophthalmology. 2022;129(2):233-5. |

