 |
|
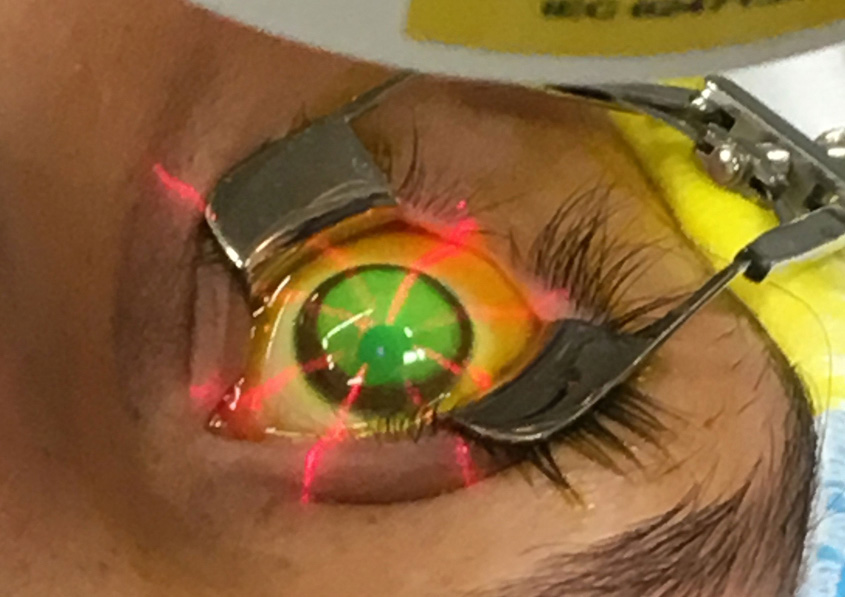
The researchers found geographic variability in CXL use and speculated that it may be linked to different environmental exposures contributing to disease severity or practice patterns of the procedure’s adoption throughout the country. Insurance coverage was a limiting factor regardless. Photo: Glaukos. Click image to enlarge. |
Since corneal crosslinking (CXL) received FDA approval in 2016, it has proven to be a revolutionary, less invasive way to prevent keratoconus progression and delay need for penetrating keratoplasty. But has adoption fallen prey to the same constraints that often limit access to healthcare in the US—namely, insurance and income disparities? Given CXL’s increasing popularity, University of Pennsylvania researchers wanted to explore whether socioeconomic factors contribute to the likelihood of patients receiving the treatment.
Included in their retrospective study were 552 keratoconus or corneal ectasia patients who had undergone CXL and 2,723 matched controls who did not undergo the procedure. The researchers were able to determine that an age of 30 years or older was associated with decreased likelihood of undergoing CXL. Encouragingly, sex, race, education and patient income were not linked with odds of receiving the treatment, but patients with health maintenance organization (HMO) insurance types did have lower odds of receiving CXL. Similarly, lower odds were seen geographically for patients who lived on the East Coast and in the lower Midwest.
The age association is a function of the natural history of keratoconus. Progression generally stops around age 40, or after 20 years since diagnosis. As such, people closer to that age, or after the age of 30, as seen with these results, would potentially make CXL less likely to happen in older, more stable patients. Furthering this association may be that older adults who would now be CXL candidates may have already received penetrating keratoplasty, thus reducing the pool of potential CXL patients. While there was no observed link of receiving CXL with sex or race, there was a trend of Hispanic and Asian patients having decreased odds of receiving CXL over white patients.
Since CXL’s US introduction, 95% of the commercially insured population now has coverage for the procedure. Related to this, income itself was not linked with crosslinking uptake, but type of held insurance was. Mainly, those with an HMO plan were less likely to receive CXL than those with better coverage. As the authors describe, an HMO requires patients to use a local network of doctors and they must seek approval from their primary care physician for specialist visits. Since physicians often need to provide objective criteria for insurance companies to approve CXL (regardless of plan type) the authors suspect patients are limited through access to see an eyecare provider to gain the needed criteria, such as Kmax or myopia/astigmatism progression.
The researchers note that CXL is complex in its likelihood of application to any given case. But, they add that “physician awareness, however, is the first step to ensuring equitable care for patients. On a larger scale, based on our results, promoting insurance companies to provide patients with easier access to specialists and ‘out of network’ physicians have the potential to help bridge both the geographic and insurance related gaps in care.”
Gupta AS, Yu Y, Orlin S, VanderBeek BL. Real world socioeconomic determinants of corneal crosslinking in a national cohort. J Cataract Refract Surg. October 13, 2023. [Epub ahead of print]. |

