 |
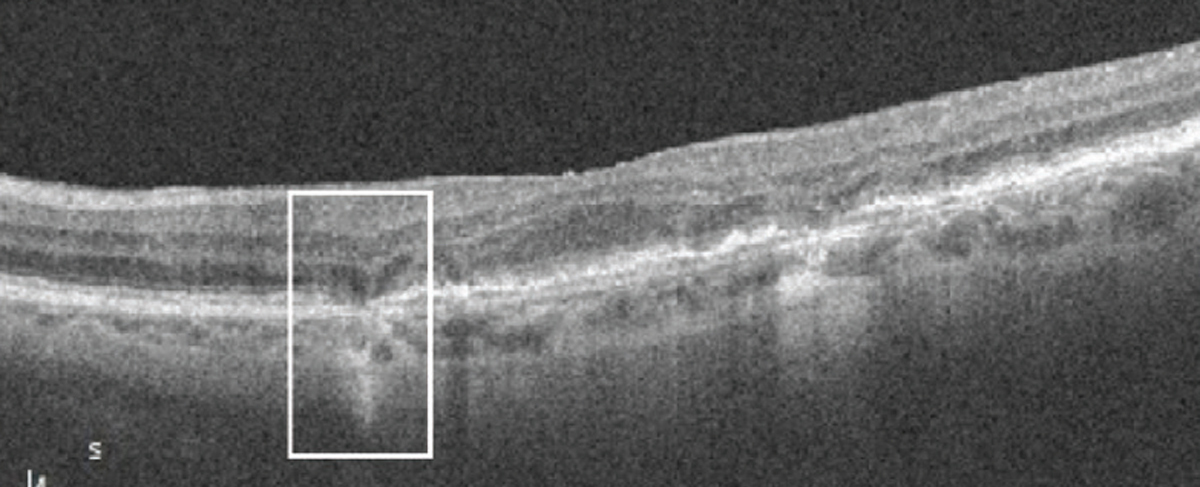
Researchers identified the following four imaging predictors of late-stage AMD development, from most to least significant: iRORA (seen here, white box), EZ status, drusen area and presence of hyperreflective foci. Photo: Anna Bedwell, OD. Click image to enlarge. |
It’s well known that patients with intermediate age-related macular degeneration (iAMD) are at risk of disease advancement, though rates of progression vary widely. While no specific anatomic markers exist to identify patients with the highest risk, a team of researchers sought to change that by performing a study on individuals with iAMD who were examined over two years. They observed two imaging findings that were associated with a higher risk of progression to late-stage disease: incomplete retinal pigment epithelial and outer retinal atrophy (iRORA) and ellipsoid zone (EZ) disruption.
The prospective study reviewed the OCT parameters of 135 patients with iAMD at baseline and the end of the 24-month follow-up period. Nearly one-third (30.4%) of patients developed advanced-stage AMD during this time. Using a risk prediction model, the researchers found that the following factors had the greatest effect on progression risk: iRORA, EZ status, drusen area and presence of hyperreflective foci. Of these, the presence of iRORA and EZ disruption conferred the highest risk of late AMD development, especially when appearing simultaneously.
“The individual predictor, iRORA, was found to account for approximately 31% of the variability observed in disease progression,” the researchers explained in their study, noting that this finding suggests iRORA is the most influential predictor variable. “The addition of three more variables, specifically the EZ disruption variable, contributed to a 5% increase in the overall explanatory power of the model, which led to more accurate predictions,” they added.
The prediction model used in this study was unable to accurately distinguish between the progression risk of specific subtypes of advanced AMD (complete RORA or nAMD). The researchers explained in their paper that the model “correctly identified four of five patients whose disease had progressed to cRORA but failed to correctly identify (0/3) nAMD patients in a randomly selected testing set.” This observation could be attributed to the fact that the SD-OCT variables in this study relate more to atrophic than neovascular features. In future studies, the authors suggested that adding vascular parameters on OCT angiography to the model may help increase its sensitivity and improve the ability to predict nAMD.
These findings propose that the combination of iRORA and EZ disruption likely constitutes a high risk of progression to advanced-stage AMD within two years in patients with intermediate disease. “We aim to continue to develop a scoring system that may facilitate general ophthalmologists in the identification of patients with iAMD with a high risk of progressing to advanced stage of disease,” the researchers concluded. “Quantifying markers of pathological retinal aging predictive of individual progression to advanced AMD is an appealing goal toward personalized risk assessment in AMD.”
Flores R, Fradinho AC, Pereira RS, et al. Identifying imaging predictors of intermediate age-related macular degeneration progression. Trans Vis Sci Tech. July 3, 2023. [Epub ahead of print]. |

