 |
Slit lamp biomicroscopy is an integral aspect of any standard ocular examination, whether routine or problem-focused. The slit lamp portion of an exam allows the clinician to evaluate anatomical structures and clinical features of pathologies that would otherwise be missed without magnification. The biomicroscope’s utility comes not only from its ability to magnify, but also in its various illumination modalities. Each serves a unique viewing purpose and is based on the relationship between ocular structures and lighting techniques.
One often-underused slit lamp technique is retroillumination; mastering this technique and applying its refractive principles can help our examinations become more effective and efficient.
Clear the Way
Retroillumination is an indirect lighting technique used in slit lamp examination to assess the integrity and clarity of the cornea and crystalline lens by examining light reflected from posterior structures. Since both the cornea and lens are intrinsically clear in the absence of pathology, regular direct illumination techniques can be difficult to use for a thorough examination.
There are two main methods and procedures to achieve retroillumination:
- Iris retroillumination. Dim the room lights to optimize contrast for retroillumination and adjust the slit lamp. The slit beam should be narrow, around 0.2mm, and defined. The height of the beam should be slightly longer than the pupil to allow enough light to pass through. Position the light source temporally, about 45.° To use iris retroillumination to examine an area of the cornea, the light beam should reflect off the iris while focus remains on the cornea; the reflected light from the iris will make subtle changes and opacities in the cornea more apparent.1,2
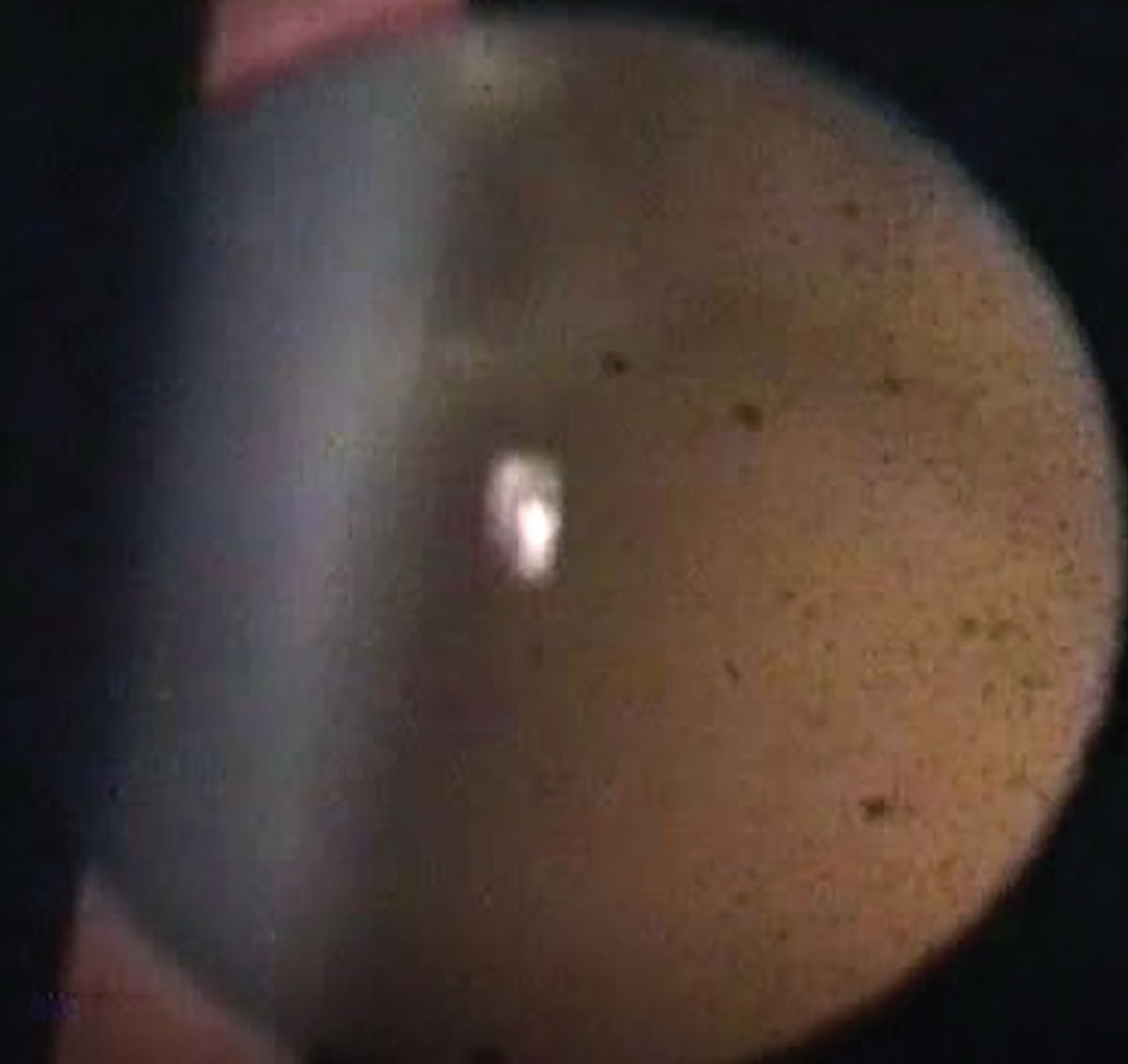
- Fundus retroillumination. Using retroillumination from the fundus, the light beam and microscope are positioned along a similar axis and the light beam is adjusted to shine through the edge of the patient’s dilated pupil. The light then passes through the pupil and into the fundus, creating a background glow. Using the red reflex or glow, opacities in all layers of the lens, as well as corneal opacities, are more easily distinguishable by the shadows they cast. If this procedure is performed through an undilated pupil, it is a way to check for iris transillumination defects.1,2
The ability for retroillumination to serve as an effective examination technique is best explained through the properties of refraction. Abnormalities within clear structures, such as the cornea and lens, are made apparent because of their interference with the emanating light as well as their refractive nature. Objects or opacities that have a higher or lower refractive index than that of their surrounding space will be distinguishable. There are two main effects that an object or opacity can elicit—acting as a diverging refractor or a converging refractor. If the abnormality embedded within the cornea or lens has a lower refractive index, it acts as a diverging lens. Conversely, that which possesses a higher refractive index than its medium would act as a converging lens.3
As a general example, the cornea possesses a high refractive index, higher than that of the aqueous. The corneal epithelial layer has a higher refractive index than the stroma. Opacities that arise within the cornea, such as blood vessels, striae and cysts, differ in refractive indices and are consequently made visible through retroillumination techniques.3
 |
|
Retroillumination using the background glow of the fundus, revealing dark opacities. Click image to enlarge. |
Another important principle in the visibility of pathologies using retroillumination is the projection or displacement of the abnormality. Whether the abnormality causes a displacement from the cornea and into the anterior tear film or posteriorly into the aqueous, it will enter an area of different refractive index, causing alterations in illumination. A clinical example would be bullae in the corneal epithelium.3
Prime Uses
Corneal dystrophies, such as posterior polymorphous corneal dystrophy, are best visualized using retroillumination, elucidating the classic peau d’orange that is commonly seen with this condition.4 The clinical use of retroillumination extends beyond optimizing an anterior segment slit lamp examination. In more recent years, it has been used in photography to enhance the identification and progression of corneal disease. Retroillumination photography analysis has demonstrated more accuracy in the grading and classification of patients with Fuchs’ endothelial corneal dystrophy.5
In addition to corneal opacities and irregularities, retroillumination focusing on the lens has long been established as the primary method of cataract grading. The Lens Opacities Classification System III is widely used today, consisting of five retroillumination images corresponding with various degrees of posterior subcapsular cataracts as well as five retroillumination images corresponding with various degrees of cortical cataracts. In clinical practice, the quantifiable grading of a patient’s cortical and capsular cataracts are not permissible without a lens evaluation using retroillumination.6,7
More recently, slit-beam associated retroillumination (SBAR) has been used in anterior segment surgery. A challenge associated with phacoemulsification is in patients with coexistent corneal opacities. To improve visibility and surgical outcomes, SBAR has demonstrated improved images and contrast through the opacified cornea, assisting in clarity during phacoemulsification by minimizing light scatter. While this technique is both cost effective and hands-free, its limitations lie in that it is dependent on flow of the red reflex, which is necessary for retroillumination.8
Aside from its various applications in anterior segment examinations, retroillumination can also be paired with confocal scanning laser ophthalmoscopy to enhance posterior segment examinations. With the addition of retroillumination, these scanning laser ophthalmoscopies can provide “pseudo three-dimensional” images. This can be achieved through the use of the light’s reflection from chorioretinal structures.
In another mode, these instruments are capable of using infrared radiation from the chorioretinal layers to create images. This type of image is useful in detecting abnormalities that exist deep within the chorioretinal areas, including small drusen, subretinal drusenoid deposits, subthreshold laser lesions and chorioretinal changes that would otherwise be missed using various en face imaging techniques.9
The current uses of retroillumination are great. It spans many categories and is still expanding with the help of combining use of other ophthalmic instruments. Besides its emerging applications, the technique should warrant consideration to use with everyday slit lamp examinations.
Dr. Labib graduated from Pennsylvania College of Optometry, where she now works as an associate professor. She completed her residency in primary care/ocular disease and is a fellow of the American Academy of Optometry and a diplomate in the Comprehensive Eye Care section. She has no financial interests to disclose.
1. Kaur K, Gurnani B. Slit-lamp biomicroscope. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. Updated June 11, 2023. 2. Martonyi CL, Bahn CF, Meyer RF. Clinical slit lamp biomicroscopy and photo slit lamp biomicrography. Time One Ink, Michigan.1985. 3. Brown N. Visibility of transparent objects in the eye by retroillumination. Br J Ophthalmol. 1971;55(8):517-24. 4. Guier CP, Patel BC, Stokkermans TJ, Gulani AC. Posterior polymorphous corneal dystrophy. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. August 8, 2023. 5. Eghrari AO, Garrett BS, Mumtaz AA, et al. Retroillumination photography analysis enhances clinical definition of severe Fuchs’ corneal dystrophy. Cornea. 2015;34(12):1623-6. 6. Chylack LT Jr, Wolfe JK, Singer DM, et al. The Lens Opacities Classification System III. The Longitudinal Study of Cataract Study Group. Arch Ophthalmol. 1993;111(6):831-6. 7. Gali HE, Sella R, Afshari NA. Cataract grading systems: a review of past and present. Curr Opin Ophthalmol. 2019;30(1):13-8. 8. Kusumesh R, Prassan B, Ambastha A, Bhasker G, Mohan N. Slit-beam retro-illumination assisted phacoemulsification for cataract with coexisting corneal opacity. Nepal J Ophthalmol. 2020;12(23):153-7. 9. Mainster MA, Desmettre T, Querques G, Turner PL, Ledesma-Gil G. Scanning laser ophthalmoscopy retroillumination: applications and illusions. Int J Retina Vitreous. 2022;8(1):71. |

