 |
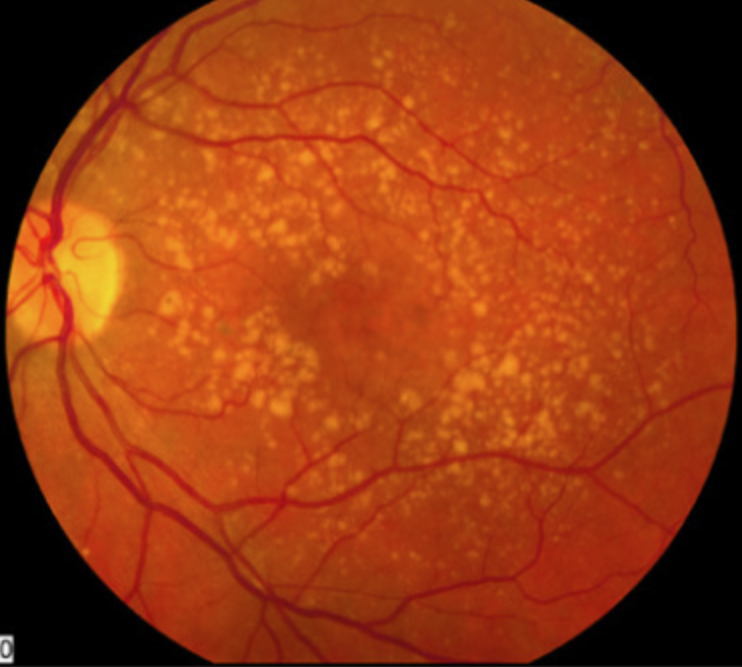
| Patients with intermediate AMD who were given 16,000 IU of Vitamin A over 90 days experienced a significant improvement in dark adaptation dysfunction. Click image to enlarge. |
Studies have suggested that a high dose of vitamin A (50,000 IU) can help improve impaired dark adaptation in patients with age-related macular degeneration (AMD). Researchers recently performed a small study to determine whether this effect persists at a lower dose of vitamin A (16,000 IU) and found that it does, but only in patients without reticular pseudodrusen (RPD). The team hypothesized that this result may indicate structural impediments to increasing availability of vitamin A in those with RPD, or, alternatively, may be reflective of the higher variability of functional parameters observed in these patients.
In the study, five patients with intermediate AMD without RPD (mean age: 78) and seven patients with RPD (mean age: 74) were supplemented with 16,000 IU of vitamin A palmitate for eight weeks. The researchers conducted assessments at baseline, four, eight and 12 weeks, including scotopic thresholds, dark adaptation, best-corrected and low-luminance visual acuities and the low-luminance quality of life questionnaire.
In those with intermediate AMD without RPD, rod intercept time improved significantly after four and eight weeks (mean change: -1.1 minutes and -2.2 minutes, respectively). The only other parameter that improved in the AMD group at the same time points was dark adaptation cone plateau (i.e., more sensitive cone threshold).
On the other hand, in the RPD group, none of the parameters improved significantly at any time point. This is despite the fact that both groups had significantly elevated serum vitamin A levels after supplementation.
“Vitamin A levels in our cohort were significantly increased after four and eight weeks of supplementation, and while they lowered after cessation of supplementation, they did not return to the baseline levels,” the researchers reported in their paper on the study, published in Retina. Similarly, the observed improvement in kinetic dark adaptation function at one and two months in the AMD group also remained significant at three months compared with baseline.
The researchers noted that this data provides evidence that “despite alterations in intermediate AMD, photoreceptors are amenable to treatment, and dysfunction can be at least partially reversed.”
However, in the presence of RPD, the team suggests that these eyes may have reached “the point of no return,” as they described it in their paper. The RPD group in this study had significantly lower rod intercept time values at baseline, which also did not improve after three months of vitamin A supplementation. “It has to be considered, therefore, that with a certain level of rod impairment, the dysfunction could be due to a loss of photoreceptors or alterations that are beyond rescue,” the researchers explained.
While the present study included just a dozen patients, its findings still have implications that in intermediate AMD, supplementing with 16,000 IU of vitamin A—a lower dose than previously studied—could partially overcome the pathophysiologic functional changes in these eyes.
Pfau K, Jeffrey BG, Cukras CA. Low-dose supplementation with retinol improves retinal function in eyes with age-related macular degeneration but without reticular pseudodrusen. Retina. June 9, 2023. [Epub ahead of print]. |

