 |
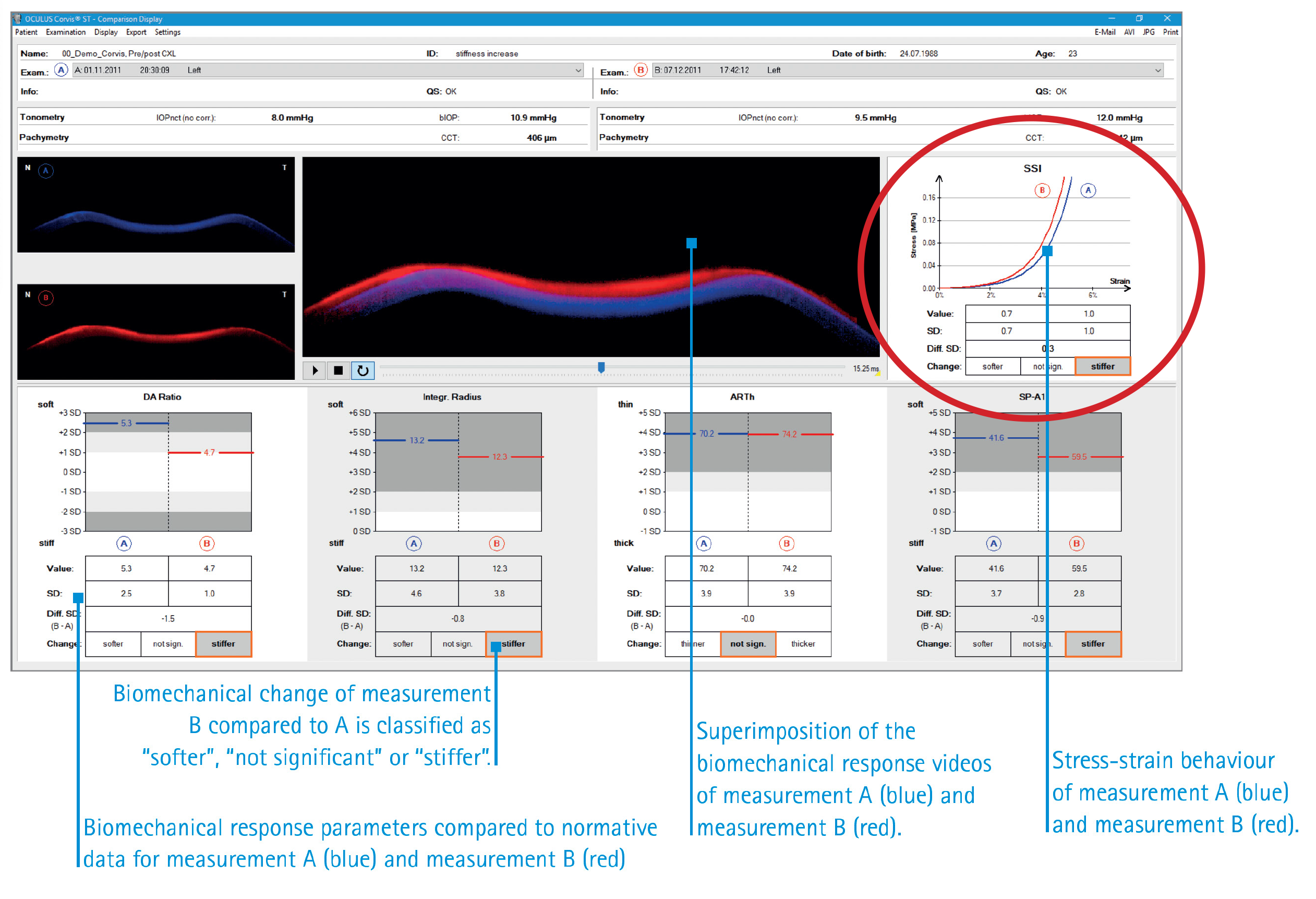
This study’s results demonstrated that some of the main Corvis ST parameters were correlated with keratoconus severity, indicating their excellent ability in classifying the condition. According to Oculus, stress-strain curves describe the elastic properties of the cornea. The curves are shifted to the right if the cornea is soft and to the left if the cornea is stiff. Photo: Oculus. Click image to enlarge. |
A parameter on the Corvis ST (Oculus) tonometer called stress-strain index was introduced to represent the influence of the cornea’s material stiffness, distinct from overall stiffness estimated by other Corvis ST parameters. The stress-strain index was recently updated to better track keratoconus progression and quantify the stiffening effect of crosslinking. Researchers of a recent study, published in American Journal of Ophthalmology, sought to assess the updated index’s ability to discriminate between normal and keratoconus corneas, as well as distinguishing different disease stages including forme fruste and subclinical types. While many of the parameters effectively distinguished severe keratoconus, only a few, such as the updated stress-strain index, integrated inverse radius, Ambrósio relational thickness and Corvis biomechanical Index performed well.
The researchers included 1,084 eyes and divided them into groups of normal (199 eyes), forme fruste keratoconus (194 eyes), subclinical keratoconus (113 eyes), mild clinical keratoconus (175 eyes), moderate clinical keratoconus (204 eyes) and severe clinical keratoconus (199 eyes). Each eye was subjected to a Corvis ST examination to determine the central corneal thickness (CCT), biomechanically corrected intraocular pressure, updated stress strain index and eight other Corvis parameters.
Before and after correction for CCT and biomechanically corrected IOP, updated stress-strain index and Ambrósio relational thickness were significantly higher, and the integrated inverse radius and Corvis biomechanical Index were significantly lower in the normal group than in the forme fruste keratoconus, subclinical and the three clinical keratoconus groups. There were also significant correlations between the values of the updated stress-strain index, Ambrósio relational thickness, integrated inverse radius, Corvis biomechanical Index and the keratoconus severity.
The area under the curve (AUC) values of the updated index for mild, moderate and severe were all over 0.95. For forme fruste keratoconus, the AUC was 0.915 with remarkable high sensitivity (79.38%) and specificity (93.47%), and a notably lower false positive rate (FPR) of 6.53%. For subclinical types, the AUC was 0.931 with sensitivity and specificity of 85.84% and 93.47%.
The authors noted that the main limitation of this study is that there was no long-term follow-up of the patients included, resulting in a lack of longitudinal verification for the biomechanical parameters to establish their diagnostic effectiveness in different grades of keratoconus.
“Further validation is needed to determine the updated stress-strain index′s potential for detecting forme fruste and subclinical keratoconus in clinical settings,” the researchers wrote in their paper. “We also encourage peer researchers around the world to perform heterogeneous testing of the updated index across races and populations to better determine its specificity, sensitivity and normal range.”
Miao YY, Ma XM, Qu ZX, et al. Performance of updated stress-strain index in differentiating between normal, forme fruste, subclinical and clinical keratoconic eyes. Am J Ophthalmol. October 23, 2023. [Epub ahead of print]. |

