 |
A 57-year-old male presented for decreased vision in his right eye for one month. He was also experiencing floaters and a general haze over the vision in that eye. Visual acuity was 20/40 OD and 20/25 OS. Intraocular pressures were 14mm Hg bilaterally, and pupils were equal and reactive without an afferent pupillary defect. His extraocular motilities were within normal limits, and he denied pain on eye movement. Color vision testing was unremarkable, as was the anterior segment exam.
In the right eye, there were four clock-hours of sectoral optic disc elevation superonasally with blurred margins (Figure 1). There was also a vitreous hemorrhage from the disc extending inferiorly. Unilateral optic disc edema was suspected.
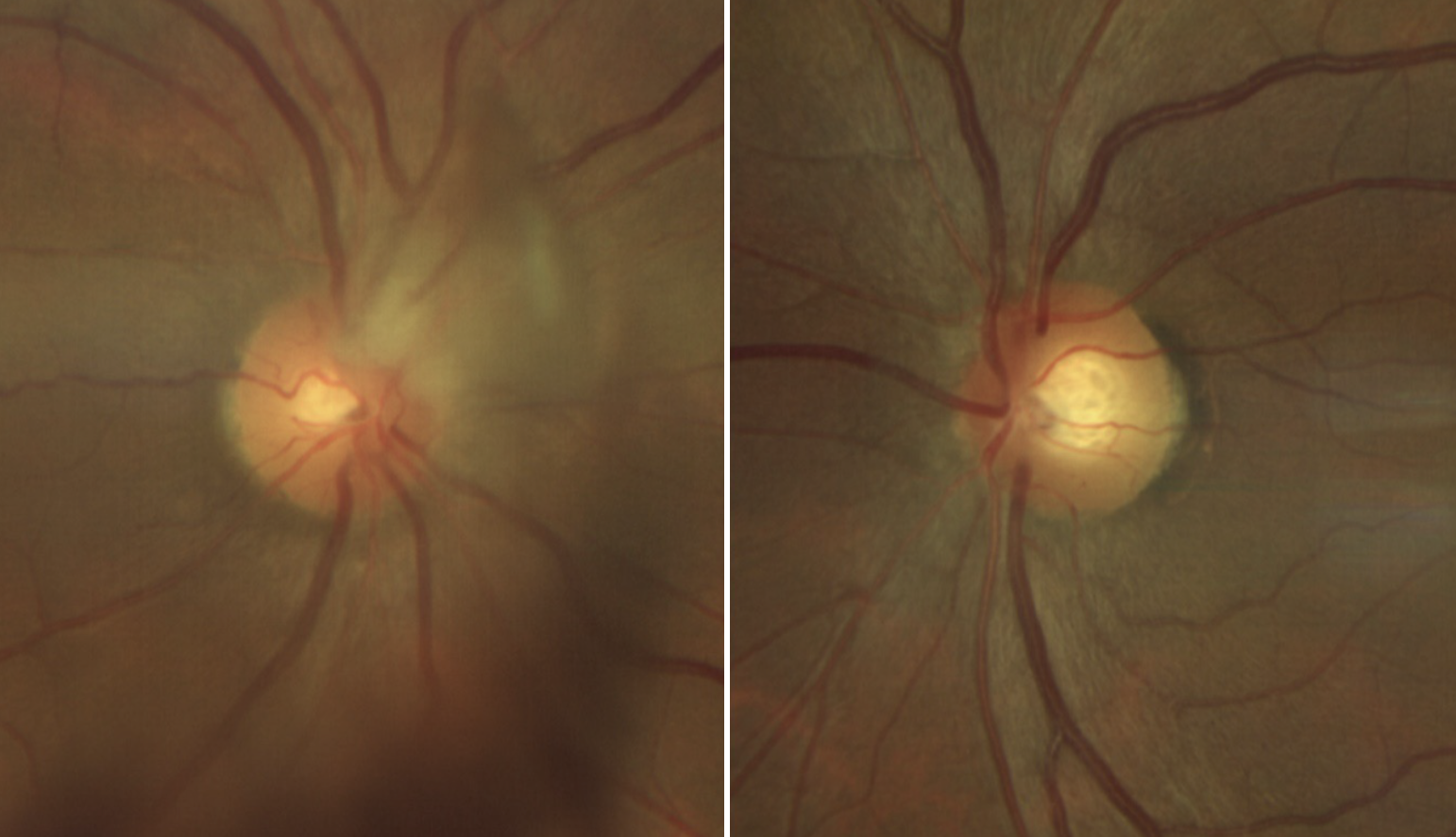 |
Fig. 1. Right and left optic nerves. The right optic nerve (left image) is seen with blurred and elevated disc margin superonasally. There is also vitreous hemorrhage causing shadowing inferiorly. Click image to enlarge. |
Edema or Not?
Optic nerve head elevation has a broad differential diagnosis usually including etiologies that result in edema, such as anterior optic neuritis, anterior ischemic optic neuropathy, increased intracranial pressure (if bilateral), diabetic papillopathy, and any condition that increases orbital congestion such as a tumor or inflammation. Buried optic disc drusen, crowded nerves and anomalous discs may also cause optic nerves to appear elevated, leading us to believe they may be edematous. These “pseudo” edema cases often pose interesting diagnostic dilemmas, as they may be difficult to differentiate from true edema.
Our patient had an initial suspected diagnosis of unilateral sectoral disc edema with hemorrhage, but how can we confirm the etiology? In this case, OCT was conducted to allow for better visualization of the optic nerve head. Both RNFL and raster studies were completed and reviewed. The RNFL study revealed thickening in the superior and nasal quadrants, as was seen clinically (Figure 2). The raster study, however, gave better insight into the morphology of the optic disc. In particular, the relationship between the vitreous and the disc was visualized. Figure 3 captures the presence of adhesion between the posterior hyaloid and the optic nerve head. This was consistent with a diagnosis of vitreopapillary traction syndrome (VPT).
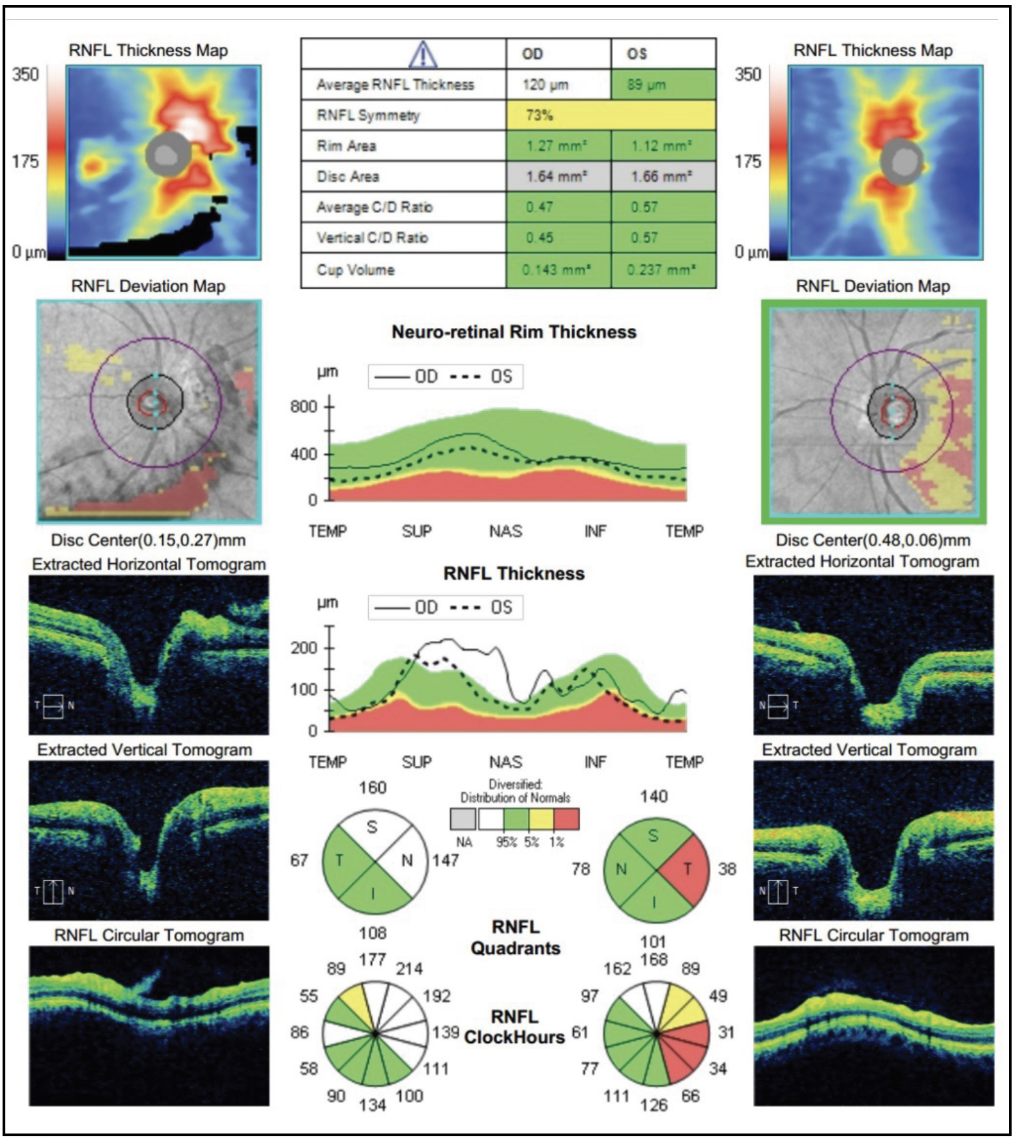 |
Fig. 2. The OCT of the RNFL is provided. The right optic nerve study reveals thickening of the superior and nasal RNFL. There is some data absent due to hemorrhage blocking signal. The left optic nerve is not elevated; there is unrelated temporal thinning. Click image to enlarge. |
In VPT, the posterior hyaloid of the vitreous body remains attached to the optic nerve head, exerting anterior traction on the disc. Clinically, this appears as optic nerve elevation and may be circumferential or partial. If it involves only part of the optic nerve head, it is usually noted superiorly.1 VPT may be seen concurrently with vitreomacular traction (VMT) or peripapillary hemorrhages and is generally unilateral, though instances of bilateral involvement have been reported. One such case involves a 47-year-old woman who was prescribed acetazolamide for one year due to an erroneous diagnosis of papilledema. She had unremarkable neuroimaging and a normal opening pressure. Eventually, OCT imaging was performed and reviewed in detail, revealing the true diagnosis of bilateral VPT.2
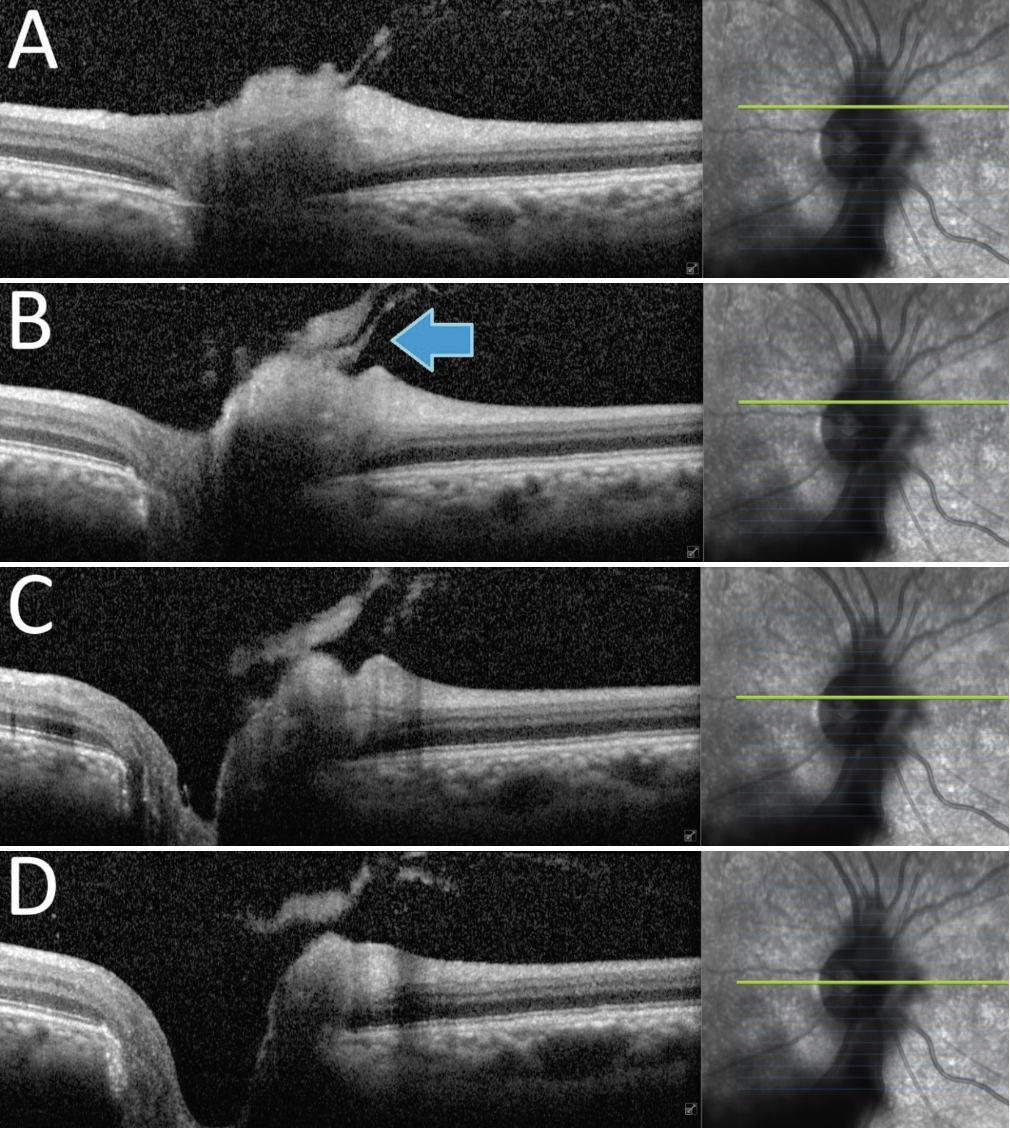 |
| Fig. 3. The raster OCT over the right optic nerve head exhibits vitreous attachment and traction on the superonasal disc margin (arrow). The hyperreflective nature of the posterior hyaloid is likely due to presence of vitreal condensation and/or blood accumulation. Click image to enlarge. |
Pathogenesis and Controversy
VPT is thought to occur, in most cases, during a posterior vitreous detachment (PVD). Recall that the vitreous has its strongest posterior pole attachments at the optic disc and macula. As the posterior hyaloid separates from the posterior pole, it often pulls away from the fovea and optic nerve head last. This leads to focal adhesion causing VMT and/or VPT. Intraretinal, subretinal or vitreous hemorrhage may also be present, as the shearing force of vitreous separation may rupture small vessels.1 Visual symptoms reported in VPT may include blurred vision, scotomas, gaze-evoked amaurosis, altitudinal defects and photopsias.3,4
Interestingly, there is discussion regarding VPT and its plausible role in the development of nonarteritic anterior ischemic optic neuropathy (NAION). Many articles suggest tractional forces on the optic disc vasculature and nerve fibers are what cause elevation of the disc, predisposing the eye to what we classically term an “ischemic” optic neuropathy. Authors suggest that maybe this “NAION” is less about ischemia and more about anatomic axonal distortion and axoplasmic flow reduction.5 A small study (n=82) found that incomplete vitreopapillary separation was present in 100% of acute NAION eyes and 92% of non-acute NAION eyes. Its authors didn’t provide the percentage of control eyes with incomplete vitreopapillary separation but cited other studies supporting that only about 68% “normal” eyes have incomplete vitreopapillary separation.6 It is something worth studying in more detail.
Treatment
Most patients with VPT are monitored with serial OCT imaging and possibly visual field testing. The condition is not generally considered to lead to prolonged visual impairment.1,7 Some cases, however, have suggested that pars plana vitrectomy may improve visual function in VPT, even with presumed NAION, but this approach is far from mainstream.8-11
Takeaways
Vitreopapillary traction syndrome has been described frequently in the literature, yet it is often misdiagnosed. Most other causes of optic nerve conditions require extensive neuroimaging and/or laboratory studies that can be costly and wasteful if done for the wrong reason. Accurate diagnosis of VPT can prevent unnecessary testing, reduce medical errors and avoid needless treatment
Dr. Bozung currently practices at Bascom Palmer where she primarily sees patients in the hospital's 24/7 ophthalmic emergency department. She also serves as the optometry residency program coordinator. Dr. Bozung is a fellow of the American Academy of Optometry and a member of the Florida and American Optometric Associations. She is a founding board member of Young OD Connect and serves on the editorial board for Review of Optometry. She has no financial interests to disclose.
|
1. Katz B, Hoyt WF. Intrapapillary and peripapillary hemorrhage in young patients with incomplete posterior vitreous detachment. Signs of vitreopapillary traction. Ophthalmology. 1995;102(2):349-54. 2. Houle E, Miller NR. Bilateral vitreopapillary traction demonstrated by optical coherence tomography mistaken for papilledema. Case Rep Ophthalmol Med. 2012;682659. 3. Nomura Y, Tamaki Y, Yanagi Y. Vitreopapillary traction diagnosed by spectral domain optical coherence tomography. Ophthalmic Surg Lasers Imaging. 2010;41:74-6. 4. Katz B, Hoyt WF. Gaze-evoked amaurosis from vitreopapillary traction. Am J Ophthalmol. 2005;139(4):631-7. 5. Parsa CF, Hoyt WF. Nonarteritic anterior ischemic optic neuropathy (NAION): a misnomer. Rearranging pieces of a puzzle to reveal a nonischemic papillopathy caused by vitreous separation. Ophthalmology. 2015;122(3):439-42. 6. Li D, Sun S, Liang J, et al. Papillary vitreous detachment as a possible accomplice in non-arteritic anterior ischaemic optic neuropathy. Br J Ophthalmol. 2023;322726. 7. Hedges TR, Flattem NL, Bagga A. Vitreopapillary traction confirmed by optical coherence tomography. Arch Ophthalmol. 2006;124(2):279-81. 8. Modarres M, Sanjari MS, Falavarjani KG. Vitrectomy and release of presumed epipapillary vitreous traction for treatment of nonarteritic anterior ischemic optic neuropathy associated with partial posterior vitreous detachment. Ophthalmology. 2007;114(2):340-4. 9. Weng CY, Khimani KS, Foroozan R, Gospe SM 3rd, Bhatti MT. A sticky situation. Surv Ophthalmol. 2018;63(5):736-44. 10. Meyer CH, Schmidt JC, Mennel S, Kroll P. Functional and anatomical results of vitreopapillary traction after vitrectomy. Acta Ophthalmol Scand. 2007;85(2):221-2. 11. Nagesha CK, Rishi P, Rishi E. Vitrectomy for vitreopapillary traction in a nondiabetic 16-year-old girl. Oman J Ophthalmol. 2017;10(1):38-9. |

