 |
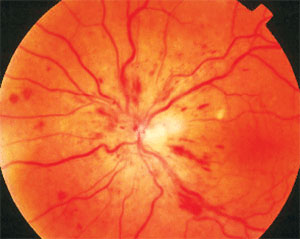
| OCT may be used to grade level and severity of macular infarction in patients with retinal vein occlusions. Photo: Joseph W. Sowka, OD. Click image to enlarge. |
A recent clinical cohort study sought to determine whether the anatomic level and severity of infarction on OCT could be used to predict long term visual acuity outcomes in eyes with central or hemi-retinal vein occlusions (CRVO or HRVO) following macular edema treatment with anti-VEGF therapy.
Data showed that individuals with more severe macular infarction at month one had worse visual outcomes despite significant improvements in macular edema. This finding suggests, according to the study authors, that macular infarction may have an impact on visual acuity following anti-VEGF.
This post-hoc secondary analysis of the phase 3 Study of COmparative Treatments for REtinal Vein Occlusions 2 (SCORE2) clinical trial included 310 of the 362 participants with macular edema secondary to CRVO/HRVO that were randomized to receive injections of aflibercept or bevacizumab.
The following grading system was used to analyze Month 1 (M01) OCT images: no infarction (grade 0), only middle retinal infarction (grade 1), diffuse middle and patchy inner retinal infarction (grade 2) and diffuse middle and inner retinal infarction (grade 3).
The study authors then correlated visual acuity letter score (VALS), central subfield thickness and number of anti-VEGF injections with the infarction severity grade at Month 1. Among the patients included in this analysis, 46 were grade 0, 5 were grade 1, 189 were grade 2 and 70 participants were grade 3.
More severe macular infarction—with both middle and inner retinal layer hyper-reflectivity (grades 2 and 3)—was associated with worse baseline (M00) VALS and was predictive of lower VALS at months 6, 12, 24, 36, 48 and 60, according to the research team.
The study also revealed an association between more severe infarction and greater central subfield thickness at presentation; however, CST decreased after anti-VEGF therapy was initiated and there was no significant difference across all grades.
“Our study supports a practical OCT grading system of macular infarction, based on the anatomic level and extent of retinal layer hyper-reflectivity, to predict visual acuity in eyes with CRVO or HRVO,” the study authors noted in their recent American Journal of Ophthalmology paper. “Specifically, eyes with worse macular infarction, as represented by hyper-reflectivity within the middle and inner retina on OCT at month 1, are more likely to have worse baseline visual acuity and worse long-term visual outcomes.
“This OCT grading scheme can therefore be used to predict long-term visual outcomes and indicates that one factor impacting long-term visual acuity may be the level of macular infarction after retinal fluid is treated with anti-VEGF,” they concluded.
Au A, Ip M, Blodi BA, et al. OCT Macular Infarction Predicts Vision in Participants with Central Retinal or Hemiretinal Vein Occlusion: A Secondary Analysis of SCORE2. Am J Ophthalmol. August 4, 2023 [Epub ahead of print]. |

