The introduction of OCT angiography (OCT-A) has allowed for noninvasive, fast and detailed imaging of nonexudative macular neovascularization (MNV) without the use of an injectable dye, easing the patient experience and expanding access to optometric practices. However, there is still no consensus on relevant OCT-A biomarkers for predicting the conversion to exudation in these eyes. Researchers in Seoul, South Korea have identified OCT-A biomarkers that could predict the near-term onset of exudation in eyes with treatment-naïve type 1 nonexudative MNV.
 |
|
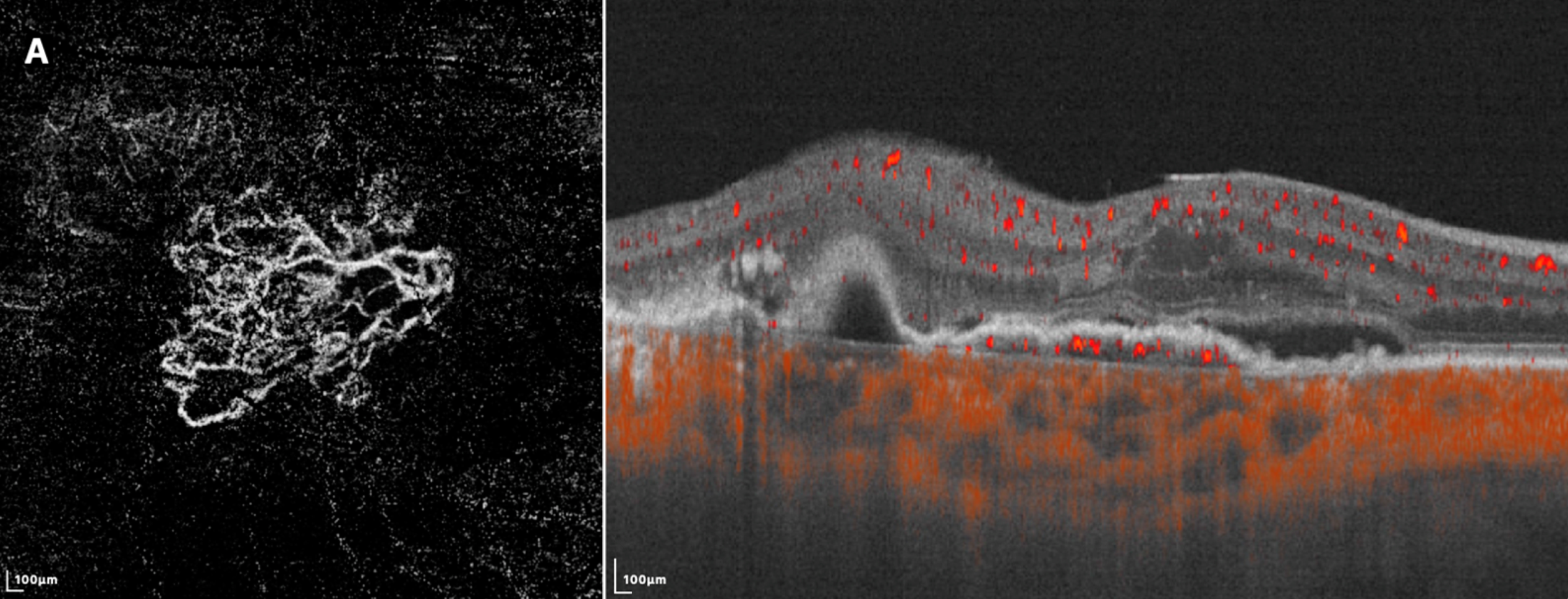
En face swept-source OCT- A (left) shows a loose pattern with characteristics such as anastomosis and loops. The corresponding B-scan SS-OCTA (right) shows subretinal fluid and rich flow signals under RPE. Photo: Gu X, et al. Diagnostics 2023, 13(14), 2458. Click image to enlarge. |
Among the morphological patterns on OCT-A known to be more frequent in active MNV, “anastomosis and loops”—an inner anastomosis between tiny vessels—was the only significant qualitative biomarker identified as useful. Among the clinically meaningful quantitative biomarkers, vessel density and junction density were significantly higher in the converted MNV group.
The retrospective study, which was published in Retina, assessed the medical records of 40 eyes. Depending on whether exudation developed within a year, the eyes were divided into two groups: active and silent. Nine developed exudation within one year, an incidence rate of 22.5%.
The active group exhibited a significantly higher rate of the anastomosis and loops pattern, greater vessel density, increased junction density, fewer number of endpoints and lower “lacunarity” compared with the silent group. Branching capillaries, peripheral arcades and hypointense halo were detected more frequently in the active group than in the silent group, although the differences were not significant.
“Our study results showing a higher rate of anastomosis, branching of capillaries and arcades at vessel termini in the active MNV group are reasonable to interpret in connection with the process of angiogenesis,” the researchers wrote in their paper.
Nevertheless, only anastomosis and loops and higher vessel density were correlated with the active group in multivariate analyses. A predictive model combining these biomarkers achieved 95% accuracy in predicting exudative conversion.
Longitudinal changes in each biomarker, such as an increase in lesion size or vessel density with disease progression, were not assessed. The researchers noted that further studies exploring these changes may suggest another scheme for predicting high-risk MNV.
“The qualitative and quantitative characteristics of nonexudative MNV in OCT-A images could help physicians evaluate the exudative risk of each patient with AMD in clinical practice,” the researchers concluded. “For eyes with a high risk of exudative conversion, more frequent follow-ups are recommended so that anti-VEGF therapy can commence as soon as symptomatic exudation develops."
Bae SH, Bae K, Yoon CK, et al. Morphological biomarkers predicting exudative conversion in type 1 nonexudative macular neovascularization using OCT angiography. Retina. February 12, 2024. [Epub ahead of print]. |

