 |
A 65-year-old Caucasian female presented to the clinic as a new patient this past June with complaints of decreased vision in her right eye and that it has been blurry for the better part of a year. Her last eye examination was three years prior and her glasses, as she explained, were never ‘just right.’
Case
Medical history included systemic medications of hydralazine, carvedolol, nifedipine, bupropion, citalopram and Lumify (brimonidine tartrate, Bausch + Lomb) PRN. She reported no allergies to medications, and she had undergone LASIK surgery OU several years ago, apparently when it was first approved in the USA.
When questioned about the visual complaints, she intimated that her right eye was just not seeing well and that her last pair of glasses didn’t seem to help too much. Entering visual acuities were 20/30- OD and 20/25+ OS. Best-corrected acuities were 20/30 OD and 20/20- OS through hyperopic astigmatic correction OU. Pupils were ERRLA and there was an equivocal afferent pupillary defect OD. Extraocular movements were full in all positions of gaze.
A slit lamp exam of the anterior segments was remarkable for clear corneal flaps with pristine interfaces OU; there were no flap edge abnormalities nor epithelial ingrowth in either cornea. Angles were open OU by Van Herick estimation. Applanation tensions were 17mm Hg OD and 13mm Hg OS. Central corneal thickness readings were 504µm OD and 532µm OS.
The patient was dilated in the usual fashion with phenylephrine and tropicamide. Through dilated pupils, her crystalline lenses were characterized by incipient nuclear sclerosis OU. Close examination of her optic nerves demonstrated a cup-to-disc ratio of 0.75x0.95 OD and 0.6x0.65 OS. The neuroretinal rim in the right eye was eroded from six to 11 o’clock; there were no disc hemorrhages noted at this visit. Her retinal vasculature was characterized by grade 2 arteriolar sclerosis OU consistent with her cardiovascular picture. The macular evaluations were essentially unremarkable with fine RPE granulation, and the peripheral retinal evaluations were also unremarkable OU.
Given the findings, a diagnosis of advanced glaucoma was made OD and probable early glaucoma OS. Also, given her complaints of decreased vision in the right eye, along with the extent of neuroretinal rim damage OD, I would imagine a visual field defect most likely involving fixation was present, accounting in part to the decreased subjective vision OD. Accordingly, the patient was scheduled for a complete glaucoma evaluation.
 |
|
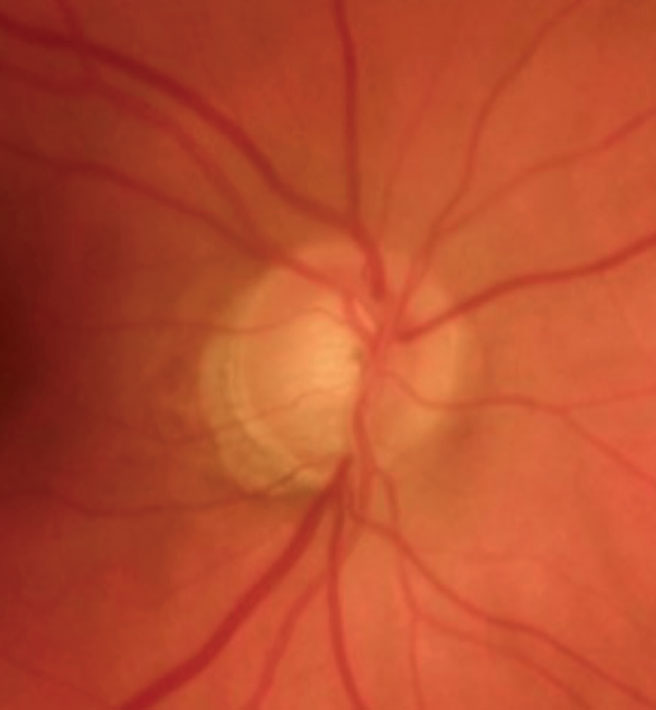
Fig. 1. The patient’s right eye in 2009. Note the thinning of the inferotemporal neuroretinal rim, calling into question the likelihood of glaucoma. Click image to enlarge. |
When discussing these findings with her, I asked if any of her previous doctors had mentioned the possibility of glaucoma with her. She said that they didn’t; furthermore, she stated that when she saw me years ago, neither did I. I was surprised by this comment, as she was registered as a new patient. Upon hearing this, my tech began looking for her previous records in our EMR; sure enough, she was seen by me in 2009.
In looking back at that visit, she had a cup-to-disc ratio of 0.5x0.7 OD and 0.5x0.55 OS with a thin, questionably eroded inferior temporal neuroretinal rim. The chart notes from that visit specifically listed glaucoma suspect OU as a diagnosis, and the patient was scheduled for a follow-up to evaluate the situation. The patient never returned to the office—until 2023.
Discussion
We’ve all seen patients on both sides of this equation. They either present as new patients with clinical findings of a long-standing condition and deny any other provider mentioned this, or they dismiss your plan of action at visitation and do not return for further care; this patient fell into both categories. How do you handle these situations?
Let’s take a look at the first scenario, in which the patient presents with advanced glaucoma—which we know has been there for a substantial amount of time. Perhaps it did develop in the interim between your visit with the patient and their previous visit by another provider, which in this case was three years earlier. In either case, we are dealing with the present situation, namely, uncontrolled normal tension glaucoma, although here, the thin post-LASIK corneas are resulting in artificially low IOP readings. As such, the situation needs to be brought under control. They need intervention of some kind, either medical or surgical.
The crux of managing glaucoma is multifactorial, but it certainly involves mitigating the risk factors for progressive optic nerve damage. But, equally important is the ‘buy in’ of the patient to your plan of action. Without it, any management plan will have a hard time succeeding, usually due to noncompliance. Of course, patient education is important, but so is a frank discussion of the potential negative effects on vision that may occur if the plan is not followed precisely and stringently.
A trusting doctor-patient relationship is not developed overnight, nor in one visit in many cases. However, that first visit is important to begin to build that sound relationship. Communication, compassion, understanding and, of course, sound clinical care are all important aspects to fostering that relationship. Unfortunately, the simple truth is that sometimes, whether the patient doesn’t understand the importance of what you’re saying, or they simply don’t want to hear it or don’t believe it, they just don’t follow through with your clinical advice, despite your best efforts. An old axiom comes to mind: a patient needs to assume a certain amount of responsibility for their own care. That holds true whether we are talking about glaucoma or diabetes, for example, or any other condition.
The second scenario is the patient who dismisses your plan of action and seeks care elsewhere. Perhaps the severity of the situation was discussed previously (as in this instance) and, for whatever reason, the patient forgot, actively ignored the advice or didn’t understand what was being said. Or, maybe even more unfortunately, a previous provider did not identify the disease process in the intervening period. In any case, it is now even more important to clear up any misunderstanding the patient may have. Firm, but clear explanations are in order here.
 |
|
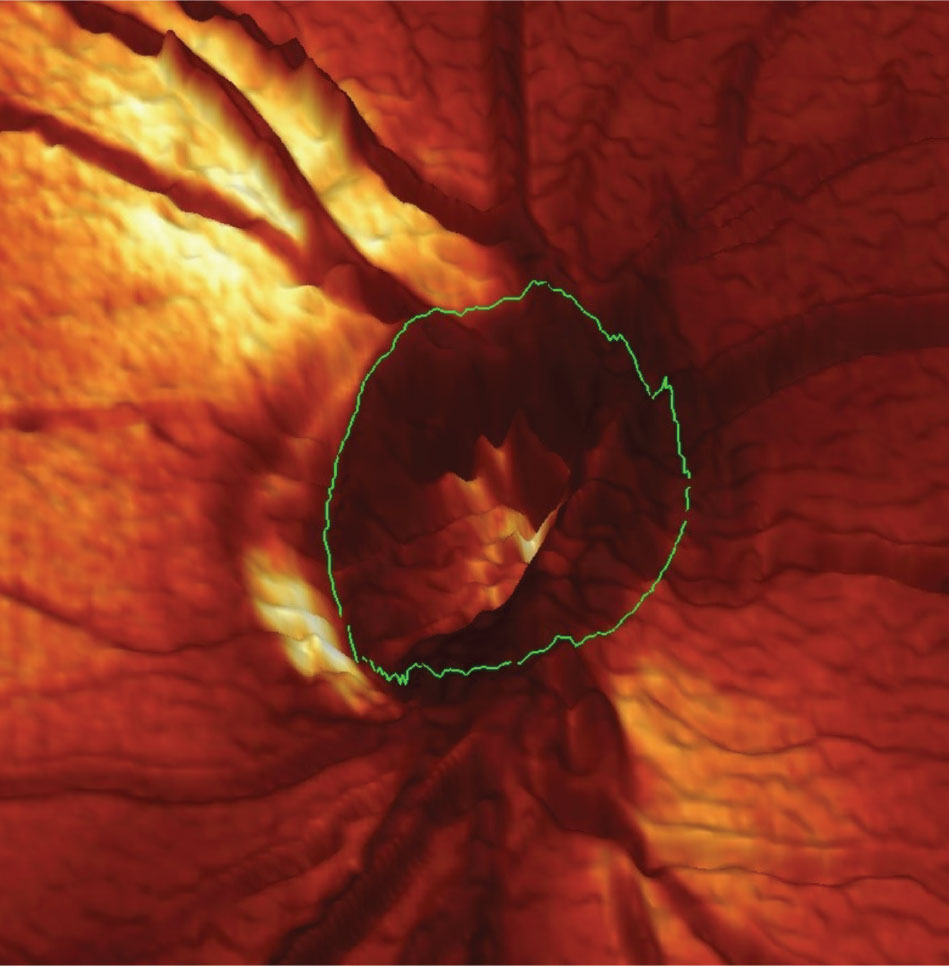
Fig. 2. This is an HRT 3 tomogram of the right optic nerve taken in 2009. Note the significant thinning and notching of the neuroretinal rim at the seven o’clock position. Moorsfield’s classification of this optic nerve at that time demonstrated a high likelihood of this sector being affected by disease rather than a statistical anomaly. Click image to enlarge. |
This then prompts the question: if they were told about this situation previously and dismissed it, why would they now act differently? In fact, I am the same provider who mentioned to the patient 14 years prior that they may have glaucoma, yet they dismissed me then—why would they not dismiss the idea now? They may, in reality, do just that, but now I have a distinct advantage. She is presenting with noticeably decreased vision in one eye, which is bothersome to her. Importantly, it is not because I said the vision was decreased but because she had noticed her vision is decreased, thus precipitating the current visit with me. Patients may deny my thought process, but they probably won’t deny their own thought process—she knew her vision has worsened.
This becomes our profession’s opportunity to be firm yet gentle with the patient. This is my second chance at the ‘first visit’ with me, in a sense. I told her at exam completion that she had glaucoma and that was playing a role in why her vision was decreased. To help foster compliance, I did mention to her that I had noticed this at our previous visit, but that she chose not to follow through with recommendations then and it is now time to start adhering to a management plan. Was this an ‘I told you so’? Not really, as in my opinion it was a way to break any lines of miscommunication or misunderstanding about the severity of her situation. Mentioning this was simply a tool to hopefully get her attention, so that I could then begin to get the situation under control.
As it turned out, we were not able to obtain structural images of her optic nerves at this particular visit due to time constraints. Unlike 14 years ago, however, the patient is scheduled for visual field and OCT imaging in a week. Her images from 2009 are presented here for completeness. Though technology has changed over the past 14 years, the imaging in 2009 was indicative of a problem. Let’s see if my second ‘first visit’ with the patient results in compliance.
Dr. Fanelli is in private practice in North Carolina and is the founder and director of the Cape Fear Eye Institute in Wilmington, NC. He is chairman of the EyeSki Optometric Conference and the CE in Italy/Europe Conference. He is an adjunct faculty member of PCO, Western U and UAB School of Optometry. He is on advisory boards for Heidelberg Engineering and Glaukos.

