 |
|
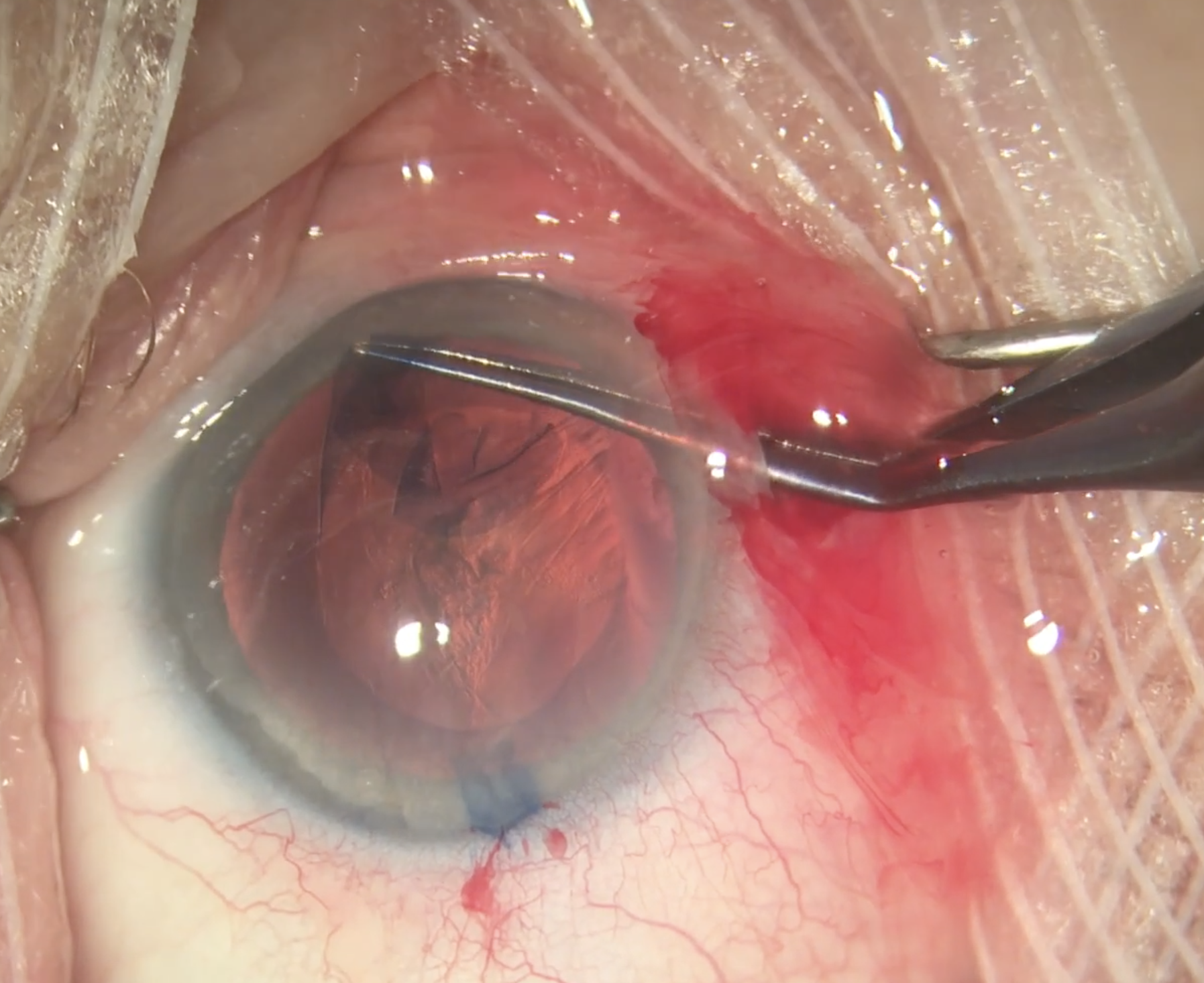
Perioperative use of IOP-lowering medications leads to significant IOP reductions following uncomplicated cataract surgery, with the largest effect associated with intracameral cholinergic or fixed-combination carbonic anhydrase inhibitor-beta-blocker formulations. Photo: Christina Tran, BS, and Leonid Skorin, Jr., DO, OD. Click image to enlarge. |
Even though intraocular pressure (IOP) spikes following cataract surgery are the most common treatable post-op complication of the procedure, there is little data regarding the optimal prophylactic regimen. In a new study, researchers investigated the efficacy of IOP-lowering medications in controlling pressure after uncomplicated cataract surgery. They found the two best options to be intracameral cholinergic use at the time of surgery or a topical fixed-combination carbonic anhydrase inhibitor/beta-blocker (e.g., Cosopt, Thea Pharma).
A total of 2,909 eyes were included from the several databases. The primary outcome was the weighted mean difference of IOP at two to eight hours, 12 to 24 hours and one to seven days postoperatively within each medication class or common fixed-combination formulations.
There was a statistically significant reduction in IOP favoring treatment arms at two to eight hours and 12 to 24 hours, with the effect wearing off beyond one day. Between medication classes, the largest effect at both two to eight hours and 12 to 24 hours was observed with intracameral cholinergic or Cosopt, while alpha-agonists, prostaglandin analogs and topical CAIs were found to be the least effective.
Intracameral agents, such as acetylcholine and carbachol, provided excellent IOP prophylaxis. “It has been hypothesized that IOP spikes following cataract surgery result from trabecular blockage by surgical debris and retained OVD. Intracameral cholinergics improve conventional outflow via the Schlemm canal, which may explain their beneficial effect in the postoperative period,” the researchers wrote in their paper.
They found a relative weaning-off effect from alpha-agonists, showing the smallest effect size beyond eight hours postoperatively across all classes. “It is not entirely clear why this may be the case,” the authors noted. “Pharmacokinetic evaluations have shown that brimonidine has a half-life of approximately two hours. In clinical studies, maximal IOP-lowering occurs between two and three hours. Thus, it is possible that the IOP-lowering effect of these agents may wear off by the 12-hour mark.”
National guidelines could be updated based on these results, the authors suggested. “Given the frequency of IOP spikes, we recommend that all eyes undergoing routine phacoemulsification should receive prophylactic treatment, where possible,” the authors concluded. “The most practical treatment of choice would be a single dose of a topical [CAI/beta-blocker]. Intracameral cholinergic agents are also highly effective, though may be a more expensive option for routine clinical use.”
Kanjee R, Popovic MM, Salimi A, et al. Prophylaxis against intraocular pressure spikes following uncomplicated phacoemulsification: a systemic-review and meta-analysis. Eye. February 7, 2024. [Epub ahead of print.] |

