 |
|
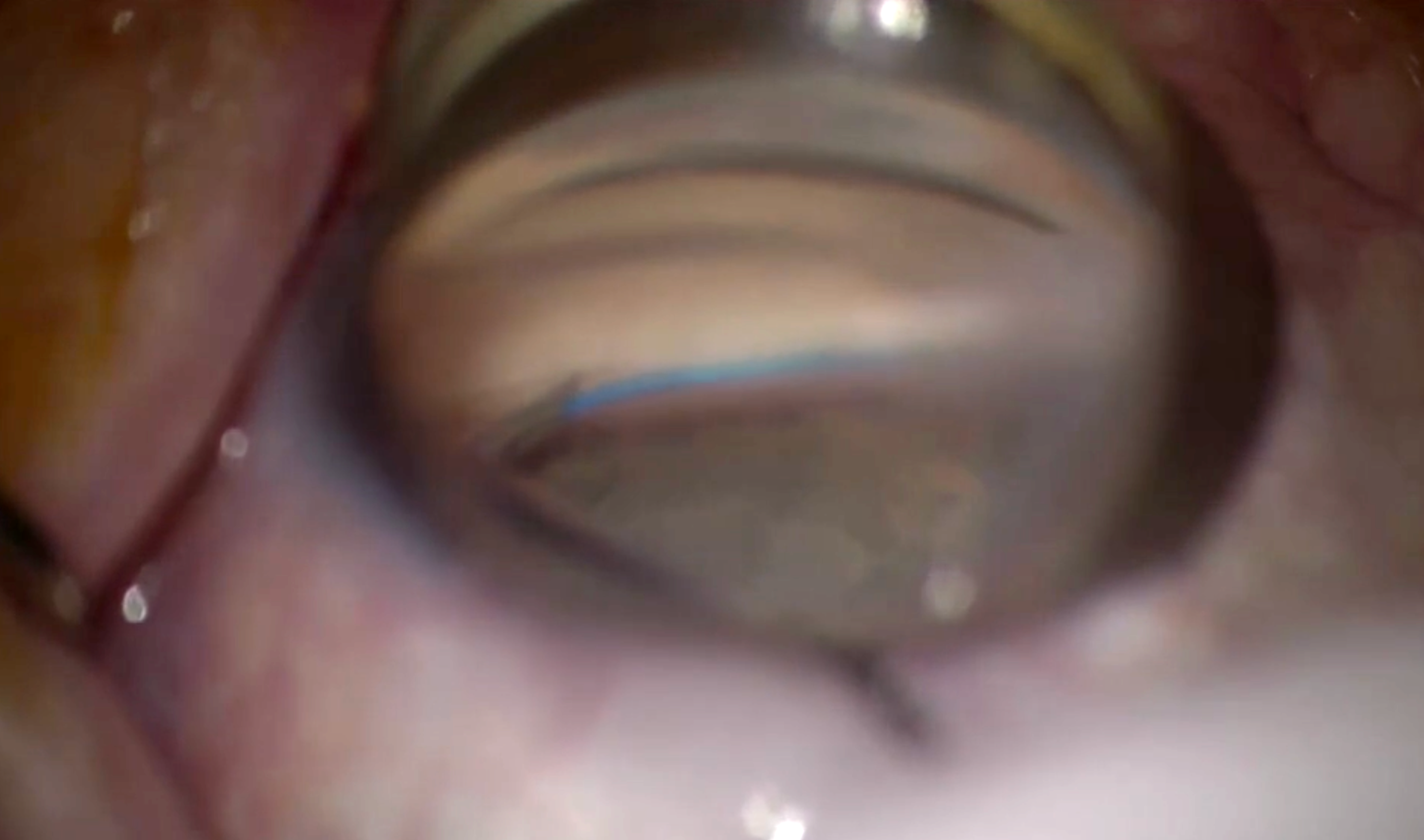
Higher baseline IOP and glaucoma secondary to medications, trauma or inflammation were also risk factors for requiring a subsequent MIGS reoperation such as goniotomy, seen here. Photo: Constance Okeke, MD. Click image to enlarge. |
Given the expansion of laser trabeculoplasty and MIGS into early—sometimes initial—glaucoma management, understanding the long-term effectiveness of MIGS procedures and identifying patients most likely to benefit from them has important clinical implications. Angle-based MIGS options (canaloplasty, goniotomy, Trabectome, iStent) have grown substantially, although long-term efficacy is poorly understood. A new study based out of Massachusetts Eye and Ear in Boston analyzed angle-based MIGS effectiveness with/without preceding laser trabeculoplasty (SLT and argon laser trabeculoplasty). The team found that, while sustained IOP reduction was seen after angle-based MIGS in all groups, eyes that had laser trabeculoplasty prior were more likely to require reoperation. Their results were published in Ophthalmology Glaucoma last Wednesday.
The study identified eyes that had undergone angle-based MIGS with/without prior SLT (< two years preceding MIGS) in the IRIS Registry over a six-year period. After propensity score matching, the study identified 954 eyes undergoing standalone angle-based MIGS and 7,522 undergoing angle-based MIGS and phacoemulsification.
For eyes only undergoing angle-based MIGS, those with prior SLT were more likely to undergo reoperation vs. those without laser trabeculoplasty at six and 12 months. In multivariate models, subjects with prior SLT were more likely to undergo reoperation over the 36-month period vs. those without it (adjusted hazard ratio: 1.53). For eyes undergoing ab-MIGS + phacoemulsification, those with prior laser trabeculoplasty were more likely to undergo reoperation vs those without laser trabeculoplasty at 12, 24 and 36 months. The researchers also identified that baseline IOP and glaucoma secondary to medications, trauma or inflammation were associated with higher hazard ratios for reoperation.
“Our work highlights the importance of understanding populations most likely to benefit from this type of MIGS and plays a role in informing treatment decisions, managing expectations and directing future research,” the researchers wrote in their paper. “While laser trabeculoplasty may provide initial IOP control, angle-based MIGS following prior laser trabeculoplasty may provide suboptimal results and the need for further surgery. Such information is useful in managing both surgeon and patient expectations.”
Mitchell W, Yang SA, Ondeck C, et al. Effectiveness of angle based minimally invasive glaucoma surgery after laser trabeculoplasty: an analysis of the IRIS Registry. Ophthalmol Glaucoma. March 20, 2024. [Epub ahead of print]. |

