 |
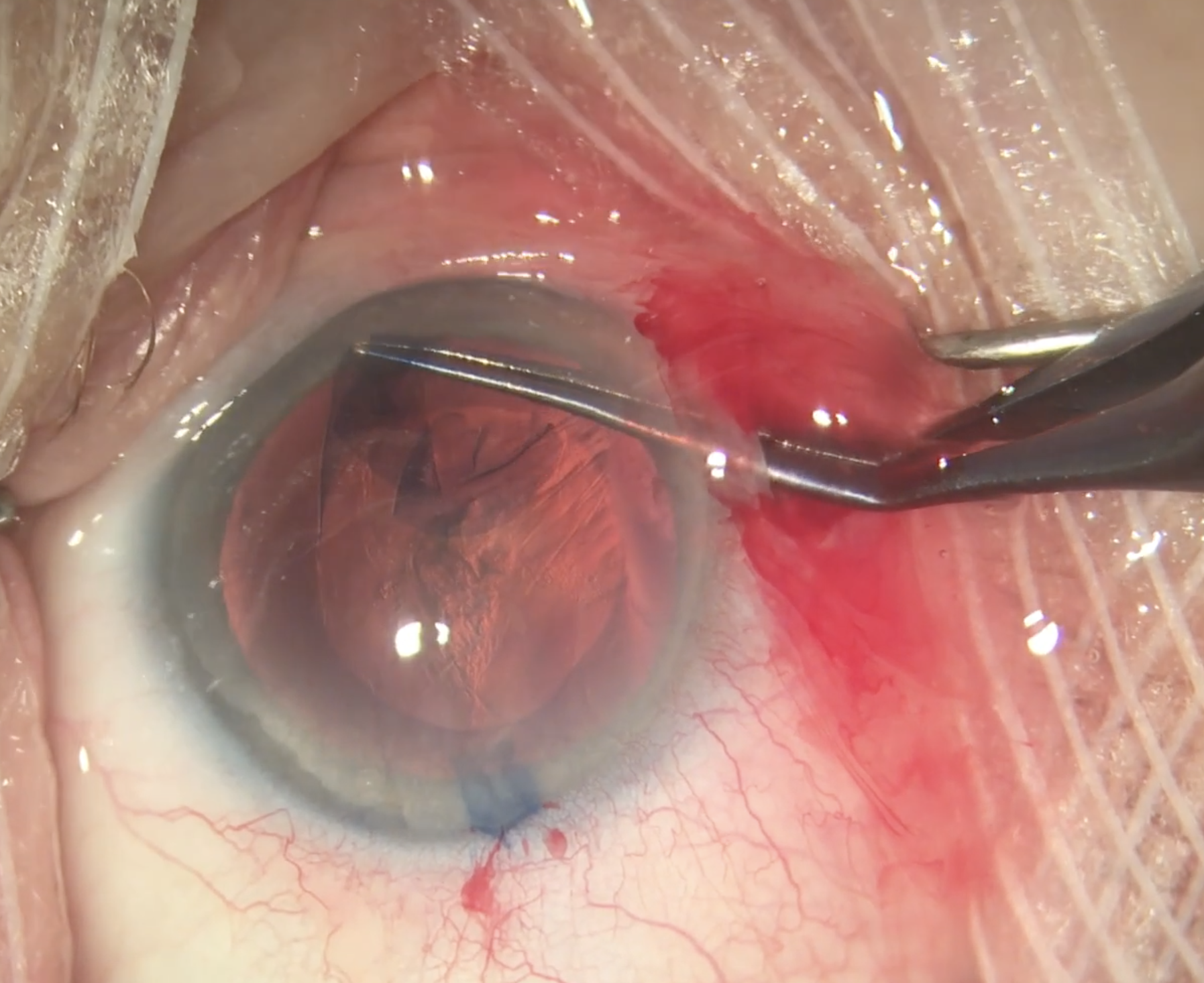
| When evaluating the pooled effect of soft vs. standard steroids on post-cataract surgery IOP in the current study, no significant difference was found between the groups. Photo: Christina Tran, BS, and Leonid Skorin, Jr., DO, OD. Click image to enlarge. |
Cataract surgery is known to induce varying levels of postoperative anterior chamber inflammation, which subsides gradually with time and appropriate anti-inflammatory treatment. It is widely assumed that the higher the anti-inflammatory potency of the steroid, the greater its ability to cause additional undesirable ocular adverse effects, of which the main concern is increased IOP. A recent meta-analysis, published in Ophthalmology, assessed the effectiveness and safety of two sub-groups of topical steroid drops, standard (prednisolone acetate 1% or dexamethasone 0.1%) vs. soft (fluorometholone 0.1% or loteprednol etabonate 0.5%), in the postoperative management of cataract surgery-induced inflammation. The team of researchers found no significant difference between the groups.
Individual study data was extracted and evaluated in a weighted pooled analysis including grading of total anterior chamber inflammation, anterior chamber cells, anterior chamber flare, postoperative visual acuity (VA), IOP and rate of adverse events. The researchers found 508 studies, of which seven were eligible for the systematic review, and were ultimately included for analysis, reporting on 593 patients from five countries. The age of included patients, when available, ranged between 3.7 to 73.4 years. Follow-up data was available for analysis at one, seven and 28 days postoperatively.
Except for a significantly lower grade of anterior flare in the standard steroid group at day seven (standardized mean difference, SMD, 0.26), inflammatory activity measurements displayed insignificant differences at every other follow-up (days one and 28 postoperatively). Pooled analysis of IOP at each follow-up demonstrated a higher IOP at the seven-day visit in the standard steroid group, whereas IOP at other time-points was comparable between the groups. Qualitative analysis of ocular adverse events showed similarities between the groups.
“It is important to base the choice of topical postoperative steroidal treatment on high-quality data regarding both risks and benefits of various drugs,” the authors wrote in their paper. “Nevertheless, safety and potency should still be considered for the individual patient with either an increased tendency for postoperative inflammation or a pre-existing glaucomatous damage to the operated eye. In the absence of such characteristics, additional factors may also influence treatment regimen choice, including cost and local availability of the topical steroids.”
Noyman DBE, Chan CC, Mimouni M, Safir M. The efficacy and safety of standard vs. soft topical steroids after cataract surgery -a systematic review and meta-analysis. Ophthalmology. November 23, 2023. [Epub ahead of print]. |

