 |
Q:
I have a patient with persistent epithelial defects consistent with neurotrophic keratitis (NK). She has failed on traditional treatments such as steroids and punctal plugs. What else can I do?
“There are many safe and effective biologic treatments for NK including amniotic membrane, Oxervate (cenegermin 0.002%, Dompe), autologous serum eye drops (ASEDs) and platelet-rich plasma (PRP),” says Hardeep Kataria, OD, of Avant Eyes Optometry & Advanced Dry Eye Center in Porter Ranch, CA. “Early NK is often misdiagnosed as moderate to severe dry eye disease due to its similarity in presentation with persistent superficial punctate keratitis (SPK),” she notes. “However, one test can differentiate dysfunctional corneal nerves: corneal sensitivity.”
A Sensitive Topic
A 66-year-old woman presented to Dr. Kataria with a longstanding history of systemic hypertension and uncontrolled type 2 diabetes with moderate nonproliferative diabetic retinopathy and diabetic macular edema (DME) in both eyes. Her medication list included insulin and antihypertensives. She had a history of intravitreal Avastin (bevacizumab, Genentech) injections and focal laser for DME.
She presented with a chief complaint of blurred vision and SPEED score of 3/28, with infrequent and mild irritation. There was no active macular edema. She admitted to having seen multiple providers who had prescribed low-dose topical steroids, cyclosporine, lifitegrast and a history of punctal plugs without improvement. She had also undergone two thermal evacuation (Lipiflow, Tear Sciences) and microblepharoexfoliation (ZEST, Zocular) procedures for severe atrophy of her meibomian glands and presence of blepharitis. Her best-corrected vision was 20/30 in each eye.
 |
|
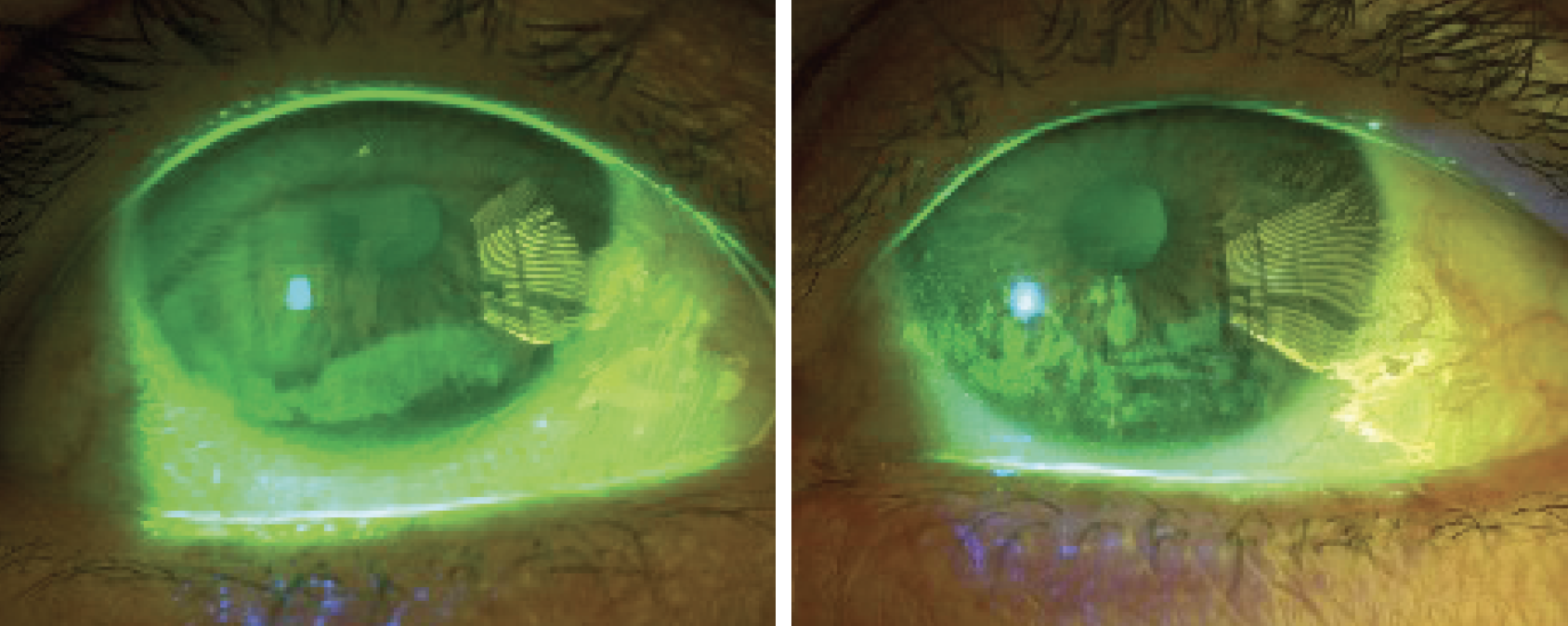
Fig. 1. OD persistent inferior corneal epithelial defect, OS persistent confluent inferior and central SPK. Click image to enlarge. |
Anterior segment examination revealed a persistent inferior epithelial defect OD and confluent SPK inferior and central OS (Figure 1). Corneal sensitivity testing with a cotton tip applicator revealed corneal anesthesia OD and hypoesthesia OS. “This corneal sensitivity points us in the direction of NK,” Dr. Kataria says.
One cryopreserved amniotic membrane was placed in each eye for three days with a temporary tape tarsorrhaphy (Figure 2). Both corneas appeared healed immediately after treatment. “Due to the progressive nature of NK, we knew that long-term treatment would be required,” Dr. Kataria notes.
Oxervate was ordered, and the patient was compliant for the typical eight weeks of treatment. The epithelial defects completely resolved, and the patient is being monitored on artificial tears.
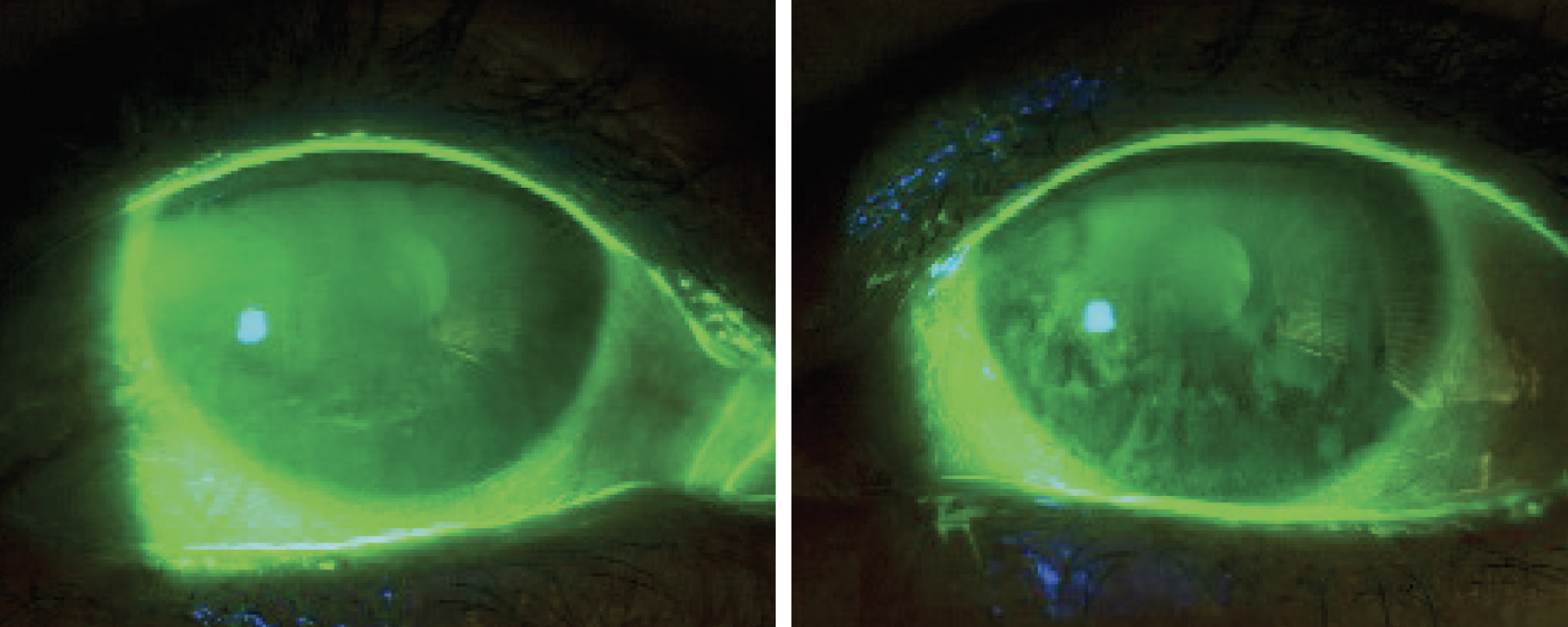 |
| Fig. 2. At left, OD improvement of epithelial defect after amniotic membrane. At right, OS improvement of confluent SPK after amniotic membrane. Click image to enlarge. |
Striking a Nerve
NK is a progressive degenerative disease of the corneal epithelium and stroma caused by damage to the corneal nerves. Maintenance of ocular surface health highly depends on a complex neuroanatomic pathway that innervates the corneal epithelium and corneal nerves.
“This mutual support promotes cellular proliferation, migration and differentiation and corneal nerve repair,” Dr. Kataria emphasizes.
Diabetic peripheral neuropathy is often seen with hyperglycemia that causes neurodegeneration and apoptosis of neuronal cells. It affects 50% of patients with diabetes, and the trigeminal nerve is no exception.1 Patients with diabetes can also present with reduced corneal nerve density as imaged on in vivo confocal microscopy, further increasing suspicions that NK can occur frequently in patients with diabetes.2
Need for Growth
Neurotrophic keratitis occurs when the corneal epithelium is persistently irregular and cannot support the corneal nerves, or vice-versa. Treatments restore the supply of neurotrophic factors to the corneal nerves and epithelium, specifically nerve growth factors. Therefore, treatments that are rich in nerve growth factors may work best, such as amniotic membrane, ASEDs, PRP and recombinant human nerve growth factor, Oxervate.
Treatment goals for early NK include promoting eyelid closure, preventing tear evaporation and improving the health of the corneal epithelium and corneal nerves. Dr. Kataria recommends using steroids and NSAIDs with caution so as to not promote superinfection and corneal melt, respectively. Punctal plugs can increase the tear lake and prevent evaporation. “Amniotic membranes, rich in nerve growth factors, are considered a first-line treatment,” she states.
Oftentimes, Oxervate requires an insurance pre-authorization that can take two weeks to obtain. Amniotic membranes work well as induction therapy until Oxervate is approved.
ASEDs and PRP are rich in neurotrophic factors and can be used as primary treatment for a persistent corneal epithelial defect.3 Sometimes, defects that are refractory to ASEDs can improve with PRP therapy.3
Oxervate has been FDA-approved for all stages of NK and is a safe and effective option to encourage corneal re-epithelialization and increase in corneal nerve density.4,5 One drop of Oxervate is instilled six times a day at two-hour intervals for eight weeks.
“Progression of NK can be sight-threatening, as deeper layers of the cornea become involved and the risk of superinfection and tissue lysis increases,” Dr. Kataria notes. “Early detection and intervention is key to preventing progression and maintaining vision.”
Dr. Ajamian is board certified by the American Board of Optometry and serves as Center Director of Omni Eye Services of Atlanta. He is vice president of the Georgia State Board of Optometry and general CE chairman of SECO International. He has no financial interests to disclose.
1. Mansoor H, Tan HC, Lin MT, et al. Diabetic corneal neuropathy. J Clin Med. 2020;9(12):3956. |

