 |  |
Following cataract surgery, patients will present for their one-day post-op visit. The exam will primarily consist of a visual acuity check, tonometry measurement and slit lamp evaluation. One finding you may come across is a hazy appearance to the cornea. What is it, and how do you act on it?
Corneal Edema
Patients will already be using their postoperative antibiotic and anti-inflammatory drops, and in most cases, this is enough. In less than a week’s time, the cornea will clear up, visual acuity will improve and no additional drops are needed. This is due to corneal edema, commonly caused by increased inflammation and intraoperative decreased endothelial cell function.1
In cases where epithelial microcysts are present, this is due to excessive corneal edema and can be caused by elevated intraocular pressure (IOP). Diligently measure the pressure, and if the patient is in pain, the secondary port can be burped to mechanically remove aqueous, lowering the IOP in-office.2 Be aware that the IOP reading will be inaccurate and typically underestimated due to the softened edematous cornea.3 In some cases, the patient may be okay to use pressure-lowering drops and monitored closely. If elevated pressures persist, treat the underlying cause (e.g., retained lens fragment, trabeculitis).
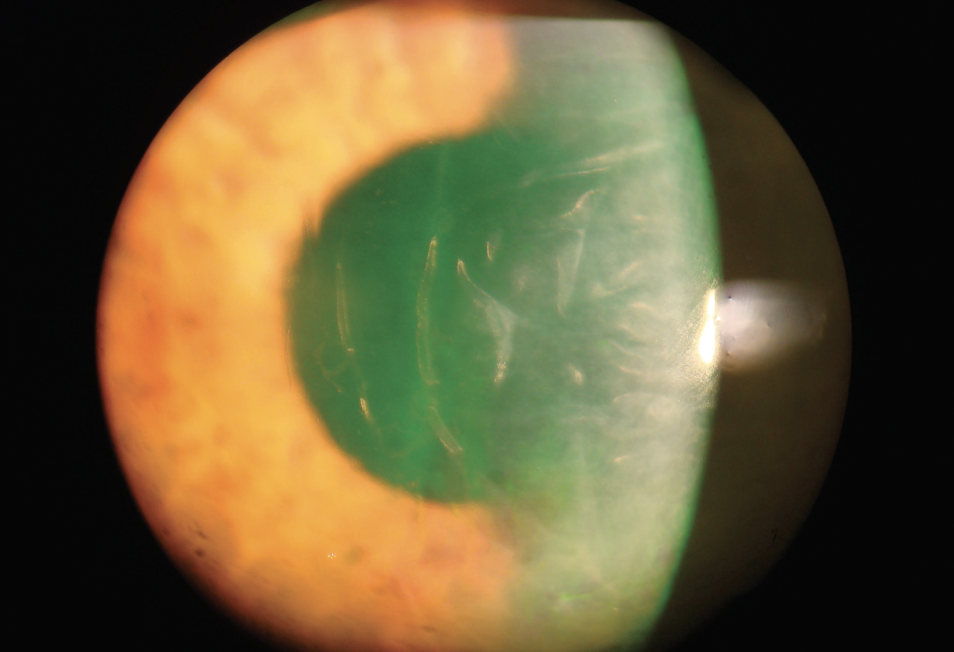 |
| Corneal swelling and endothelial folds at a one-day cataract surgery post-op. Photo: Derek Cunningham, OD. Click image to enlarge. |
The cornea’s transmissibility is possible due to the unique structural arrangement of each corneal layer. At the endothelial level, barrier and pump functions promote deturgescence and maintain tissue thickness.5 Endothelial tight junctions’ barrier function is heavily dependent on calcium and adenosine. Irrigation solutions and drugs used intraoperatively can cause insult to the pump’s ability to function and limit calcium ion availability, both of which contribute to corneal edema.2
Differential Diagnoses to Rule OutEndophthalmitis: this is usually present three to five days after surgery; corneal edema associated with lid swelling, hypopyon, vitreous exudates, blunting of red reflex and retinitis Herpetic endotheilitis: keratic precipitates, reduced corneal sensation and past history of recurrent attacks Endothelial dystrophies: prominent guttae present in fellow eye Toxic endothelial cell destruction (TECD) syndrome: significant corneal edema within 24 hours after surgery characterized by star-shaped Descemet’s folds and count fingers visual acuity Toxic anterior segment syndrome: similar to TECD, with less edema, a marked inflammatory response and an occasional hypopyon |
Intraoperative risk factors include procedural trauma from instrument use, irrigation techniques/materials and surgery duration. Inflammation and the generation of free radicals have been found to cause endothelial cell dysfunction, which has led to the use of irrigating solutions such as viscoelastic and balance salt solution. These contain sodium hyaluronate which has less impact on the calcium-dependent tight junctions.5
Pre-existing risk factors that are likely to increase the severity of corneal edema include low endothelial cell count, corneal endothelial dystrophies, iridocorneal endothelial syndrome and pseudoexfoliation syndrome. This last one which may lead to pseudoexfoliative material adhering to the corneal endothelium, which disrupts its appearance and function.2
Edema initially gives the cornea a dull and hazy appearance with the concurrent presence of increased corneal thickness. The hazy presence is not to be mistaken for residual viscoelastic, which will have a more clustered, less diffuse appearance on the posterior endothelial surface. As the edema persists, the cornea may start to reveal the appearance of microcysts, bullae and scarring.2
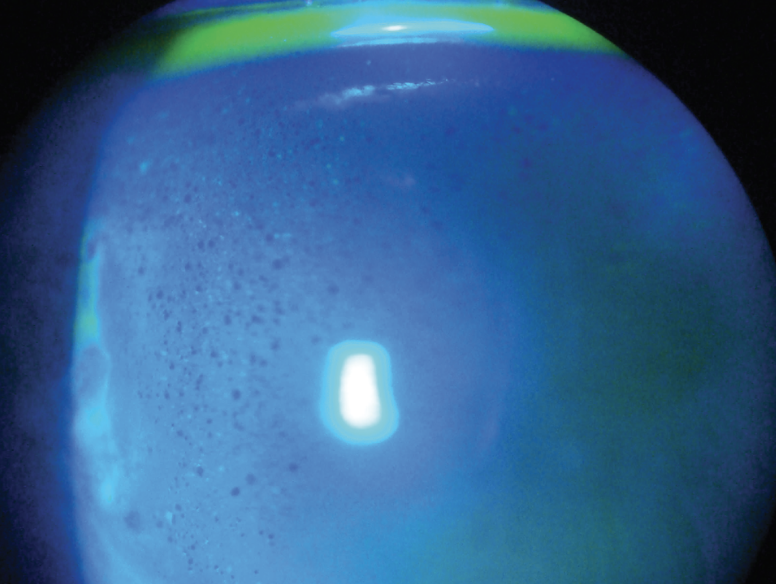 |
| Microcystic edema from corneal swelling at a one-day cataract post-op. Photo: Derek Cunningham, OD. Click image to enlarge. |
Management
This includes the use of hypertonic agents such as sodium chloride 5% eye drops to help draw water out of the edematous cornea, but doing so can lead to irritation and may have little impact in reducing stromal edema. Anti-inflammatory drops help speed up the reduction of postoperative inflammation, typically given in the form of a topical steroid.2
Surgical management is rarely required. In cases of Descemet’s membrane detachment, spontaneous reattachment is commonly seen within days following surgery. In more severe cases, surgical intervention is needed in the form of an air or gas injection. When there is severe irreversible endothelial damage, as a last resort endothelial keratoplasty or penetrating keratoplasty surgeries are performed.6
Overall, cataract and refractive lens procedures have evolved tremendously, with all the advancements and even the most proficient surgeons, postoperative corneal edema is still commonly present.2 Often, it’s self-limiting and seldom a long-term issue. A thorough preoperative consult, minimal intraoperative endothelial insult and vigilant postoperative care will assist in limiting poor outcomes and unsatisfied patients.
Dr. Cunningham is the director of optometry at Dell Laser Consultants in Austin, TX. He has no financial interests to disclose. Dr. Whitley is the director of professional relations and residency program supervisor at Virginia Eye Consultants in Norfolk, VA. He is a consultant for Alcon.
Dr. Martin is an ocular disease resident at Dell Laser Consultants in Austin, TX. He has no financial interests to disclose.
1. Díez-Ajenjo MA, Luque-Cobija MJ, Peris-Martínez C, et al. Refractive changes and visual quality in patients with corneal edema after cataract surgery. BMC Ophthalmol. 2022;22(1):242 2. Sharma N, Singhal D, Nair SP, et al. Corneal edema after phacoemulsification. Indian J Ophthalmol. 2017;65(12):1381-9. 3. Herr A, Remky A, Hirsch T, et al. Tonometry in corneal edema after cataract surgery: Dynamic contour tonometry versus Goldmann applanation tonometry. Clin Ophthalmol. 2013;7:815-9. 4. Hoffman RS, Fine IH, Packer M. Retained IOL fragment and corneal decompensation after pseudophakic IOL exchange. J Cataract Refract Surg. 2004;30(6):1362-5. 5. Narayanan R, Gaster RN, Kenney MC. Pseudophakic corneal edema: a review of mechanisms and treatments. Cornea. 2006;25(9):993-1004. 6. Sarkisian Al-Mezaine HS. Descemet’s membrane detachment after cataract extraction surgery. Int Ophthalmol. 2010;30(4):391-6. |

