 |
History
A 37-year-old man presented to the office with a chief complaint of headache via the emergency department. He explained that his vision was also poor in both eyes for the previous seven days. His ocular history was non-contributory. His systemic history was positive for hypertension, diabetes and hypercholesterolemia. He admitted to poor medical compliance. He denied trauma or allergies of any kind.
Diagnostic Data
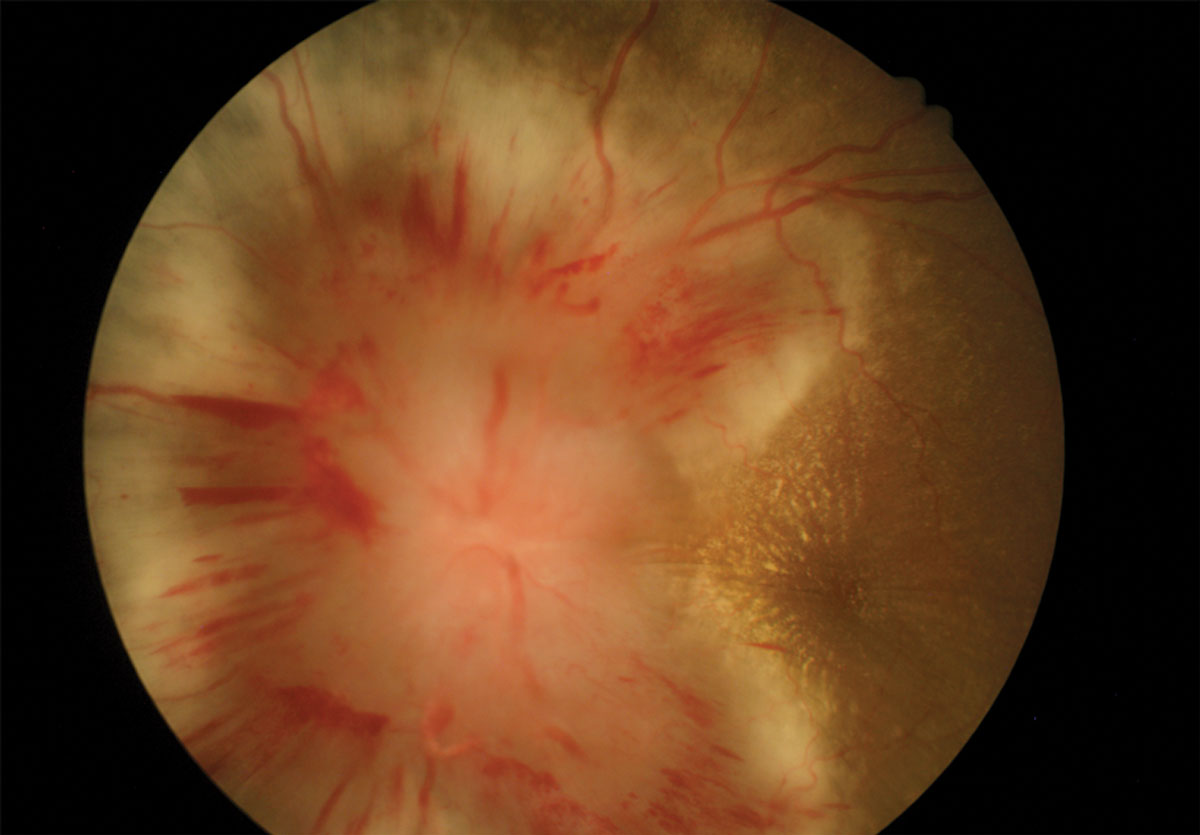
His best-corrected entering visual acuities were 20/70 OD and 20/100 OS at distance and near. His external examination was normal with the exception of facial Amsler distortion OU. There was no afferent pupillary defect. His anterior segment findings were normal. Goldmann applanation tonometry measured 17mm Hg OU. The pertinent dilated fundus examination findings are demonstrated in the photographs.
Discussion
Additional studies included optical coherence tomography of the discs to document the initial levels of disc edema. Color photography was completed to record the initial appearance of both optic nerves. Automated perimetry was completed to assess the baseline function or his retinas and discs.
The diagnosis in this issue is grade IV hypertensive retinopathy, OU. Systemic arterial hypertension causes microvascular abnormalities throughout the body producing atherosclerotic changes and end-organ damage.1-4 Hypertensive retinopathy (HR) permits the clinician to visualize ocular hypertensive changes which correlates with damage happening elsewhere in the body, particularly in the brain and kidneys.1,3,4 Retinopathy, choroidopathy and optic neuropathy are all possible complications of hypertension depending on the severity.2
 |
 |
| These fundus images show a patient’s left (above) and right eyes. Can these images explain his headaches and poor vision? Click images to enlarge. |
The effects of hypertension are demonstrated in the eye as auto-regulatory vasoconstriction with narrowing of the retinal arteriolar lumens. This is a homeostatic response to elevated blood pressure.1,3,4 In the Keith-Wagner-Baker classification scheme, this is regarded as Grade 1 HR.4,5 Grade 2 HR occurs when chronic hypertension causes focal narrowing of arterioles as well as atherosclerotic changes to the arteriolar walls.2-4 At arteriovenous crossings this manifests as nicking of the veins (also called Gunn’s sign) or deflection of the vein (Salus sign).1-5 Other atherosclerotic signs include broadening of the arteriolar light reflex and increased tortuosity.1-2,4
Acutely elevated blood pressure may overcome autoregulatory mechanisms and break down the blood-retinal-barrier.1 This causes extravasation of vessel contents.3 Splinter hemorrhages in the retinal nerve fiber layer (RNFL) and lipid exudates appear. More ominously, retinal microinfarcts (known as cotton wool spots) appear in the RNFL.2,3 Vision may be decreased from macular edema.1 These findings signify Grade 3 HR and greater risk of stroke and mortality.1,3,5
Stage 4 HR is signified by papilledema.1 A “macular star” may be seen when exudate collects in a radial pattern around the fovea.1 This represents profound failure of vascular control and can result in vision loss and death. This condition is a true medical emergency and requires immediate referral for blood pressure management. Vision loss occurs from macular edema and optic atrophy.1
Hypertension also causes constriction of choroidal vessels causing focal necrosis of the choriocapillaris and retinal pigmented epithelium (RPE). This manifests early as white areas of choroidal necrosis known as Eslchnig spots.1-2 These eventually fade and develop into focal areas of RPE hyperplasia.1-3 Subretinal fluid and serous retinal detachment may also develop in the chronic phase.1-2
In addition to macular edema and optic atrophy, HR confers a risk for retinal artery occlusion, retinal vein occlusion and retinal arterial macroaneurysm. Non-arteritic ischemic optic neuropathy (NAION) is also an associated finding.1,3,4 The presence of HR can also exacerbate diabetic retinopathy, age-related macular degeneration and glaucoma.3,4,6,7 Differentials for HR include diabetic retinopathy (or papillopathy), retinal vein occlusion, anterior ischemic optic neuropathy and neuroretinitis.1-4
The treatment for hypertensive retinopathy is controlled lowering of blood pressure. This should be accomplished in an emergency room setting where severely elevated blood pressure (>200/120) or disc edema are present. Atherosclerotic changes are permanent but arteriolar narrowing, exudates and disc edema typically resolve within months.2 Hypertensive retinopathy is also useful to assess the risk of stroke as well as congestive heart failure and renal failure.3,4 Even the presence of Grade 1 HR confers a 2-3 fold increased risk of stroke.1 Patients with HR are also at higher risk for cognitive decline, cerebral white matter lesions and cerebral atrophy.4 Untreated Grade 4 HR has a mortality rate of 50% at 2 months and 90% at 1 year.2 The optometrist’s role in this condition is recognition of the underlying systemic condition, immediate referral for appropriate management and correspondence with the internist to re-evaluate the patient’s overall health and compliance with medical therapies.
Dr Gurwood thanks Nick Karbach, OD for his contributions to this article.
|

