 |
|
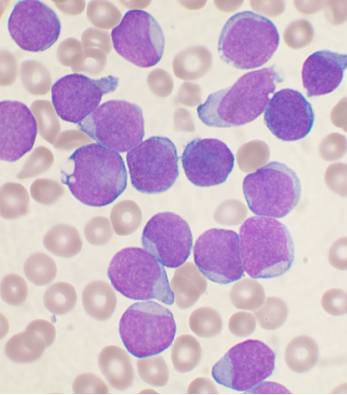
Patients in this small study with acute leukemia had significantly more hyperreflective foci than controls, though this number was reduced after remission. Photo: Vashi Donsk/wikicommons. Click image to enlarge. |
In the early stages of leukemia, cancerous blood cells may affect any organ in the body. When the disease spreads to the eye, the health of the choroid often takes the biggest hit, with nearly every case of acute leukemia presenting with choroidal infiltration. However, research is still needed to characterize these choroidal changes in vivo. One group of investigators recently sought to fill this gap in knowledge by comparing the choroidal perfusion metrics between acute leukemia patients and controls and evaluating choroidal changes before and after disease remission. They concluded in their paper in Acta Ophthalmologica that their findings demonstrated “a subclinical choroidal involvement in patients with acute leukemia, with relative stromal thickening in the acute phase and normalization after disease remission.”
The prospective, longitudinal study included a small cohort of 14 patients (26 eyes) with acute leukemia and the same number of age- and sex-matched healthy controls for cross-section comparison. For all patients (before and after remission for leukemia patients), the team performed OCT and OCT angiography and measured subfoveal choroidal thickness total, luminal and stromal choroidal area, choroidal vascularity index, choriocapillaris flow deficit density and choroidal hyperreflective foci number.
The researchers reported that the total, luminal and stromal choroidal area and choroidal hyperreflective foci number were significantly higher in acute leukemia patients than in controls. Additionally, “lower hemoglobin levels were associated with lower choroidal thickness (r = 0.58)” and “higher D-dimer values were associated with lower total choroidal area (r = -0.52), lower luminal choroidal area (r = -0.50), higher choriocapillaris flow deficit density (r = 0.41) and higher choroidal hyperreflective foci number (r = 0.47),” they noted in their paper. There were no differences in choriocapillaris flow deficit density between diseased and healthy eyes.
Ten eyes of five patients reached remission during the study period. When they were reimaged a median of four months afterward, patients had significantly reduced choroidal thickness, total and stromal choroidal area and choroidal hyperreflective foci number. The researchers also found that compared with the active phase, choroidal vascularity index increased significantly post-remission.
Based on these findings, the team speculated that choroidal hyperreflective foci can be considered a biomarker of leukemic choroidopathy, as patients with the disease had significantly more than controls, which was considerably reduced after remission. They further explained in their paper, “As leukocyte (especially macrophages) recruitment and activation occur in leukemic niches, we speculate choroidal hyperreflective foci may be leukemic or inflammatory cells.”
Recognizing that larger and longer studies are needed to further investigate the clinical manifestations of leukemic choroidopathy, the study authors concluded that using multimodal imaging, they were able to depict in vivo “the subclinical choroidal change in patients with acute leukemia, finding a predominant stromal involvement in the acute phase.”
Menean M, Apuzzo A, Mastaglio S, et al. Imaging biomarkers of leukemic choroidopathy. Acta Ophthalmologica. January 26, 2023. [Epub ahead of print]. |


