 |
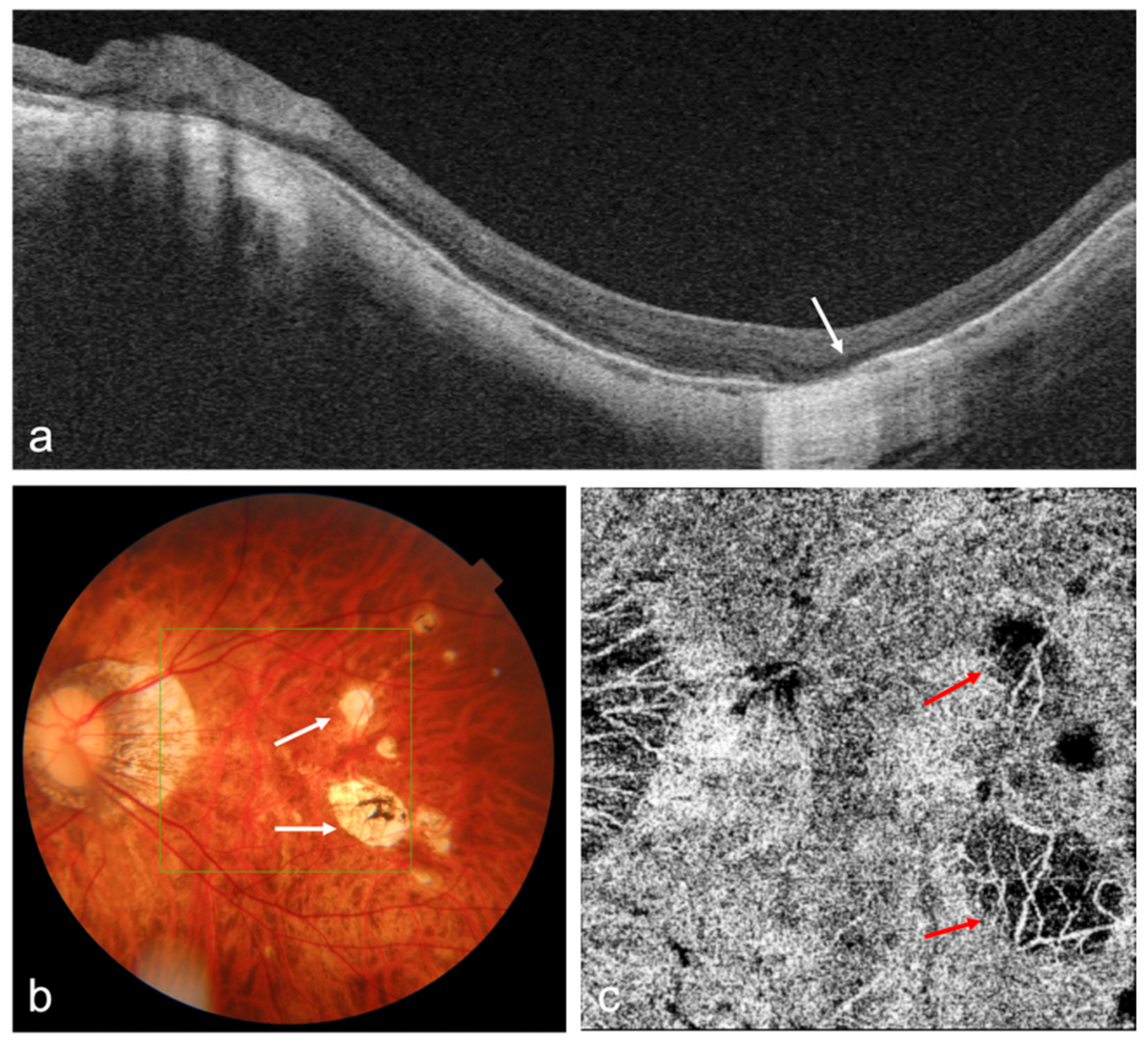
| OCT and OCTA images of a highly myopic eye with patchy chorioretinal atrophy. (a) Swept-source OCT (SS-OCT) B-scan image shows the loss of retinal pigment epithelium (RPE), Bruch’s membrane, and choroid corresponding to the patchy atrophy area (white arrow); (b) Fundus photography shows patchy chorioretinal atrophy (white arrows); (c) OCTA image shows the loss of choriocapillaris flow signals corresponding to the patchy atrophy area (red arrows). Photo: Yong Li et al. Diagnostics 2022, 12(6), 1418. Click image to enlarge. |
Previous studies have suggested that choroidal thinning plays an important role in the pathogenesis of myopic maculopathy. Researchers recently examined this association in a general Japanese patient population with different stages of myopic maculopathy and found that individuals with smaller choroidal thickness had higher risk of myopic maculopathy development.
A total of 2,841 residents of a Japanese community over the age of 40 in different stages of myopic maculopathy ranging from early to advanced were enrolled. Of this cohort, 41.4% had myopia. Choroidal thickness was measured with swept-source OCT.
Results showed that 2.9% of participants (n=81) had myopic maculopathy (45 diffuse chorioretinal atrophy, 31 patchy chorioretinal atrophy and five macular atrophy). Among the myopic individuals with axial length ≥24mm, thinner choroidal thickness was significantly associated with prevalent myopic maculopathy.
“The risk of diffuse and patchy atrophy increased significantly with the thinning of choroidal thickness levels,” the study authors noted in their paper. “Most notably, individuals with lower choroidal thickness were at higher likelihood of myopic maculopathy even if they had relatively mild to moderate myopia with axial length of 24mm to 26.5mm. Their risk of prevalent myopic maculopathy was further increased if they had both lower choroidal thickness and longer axial length of ≥26.5mm.”
Additionally, the study also revealed that lower choroidal thickness was significantly associated with diffuse chorioretinal atrophy and patchy chorioretinal atrophy, which are both observed during the early progression of myopic maculopathy.
No significant associations were found between choroidal thickness and systemic vascular risk factors known to cause ischemia in the retina, such as diabetes and hypertension.
“Taken together, these findings support the idea that the choroidal localized vasculature rather than systemic vascular change may cause choroidal thinning and may be the main player in the pathogenesis of myopic maculopathy,” the authors wrote.
Several studies have revealed that mechanical stretching stress due to the elongation of axial length can lead to rupture of the capillary network and attenuation of fibroblasts in the choroidal layer. “Therefore, our findings suggest that choroidal thinning and longer axial length may contribute to the etiology of myopic maculopathy through the choroidal vascular changes and ocular stretching stress,” the investigators concluded in their study.
Ueda E, Yasuda M, Fujiwara K, et al. Association between choroidal thickness and myopic maculopathy in a Japanese population: the Hisayama Study. Ophthalmol Sci. May 15, 2023. [Epub ahead of print]. |


