 |
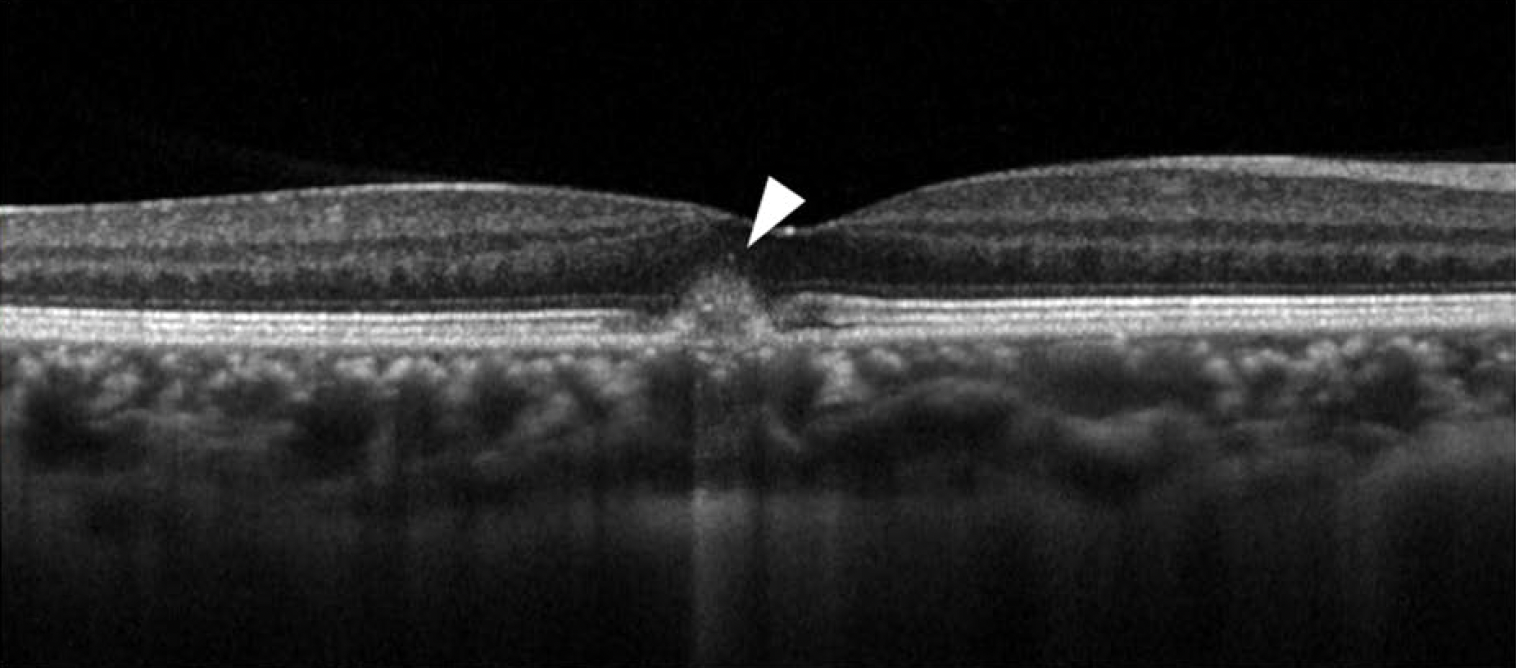
| While macular neovascularization is a common source of chorioretinal thickening, clinicians should be aware that some cases of non-neovascular pachychoroid disorder also present with hyperreflective signal on OCT. This SD-OCT of a 36-year-old woman with visual complaints in her right eye revealed a CCT of 305μm with pachyvessels. Elevation of RPE with HRM at the subretina was also observed. Photo: Maruyama-Inoue Met al. BMC Ophthalmol. June 6, 2023. Click image to enlarge. |
The relatively new disease classification of pachychoroid spectrum disorder continues to be refined by new studies and case reports. Recently, a small retrospective study included data collected from 11 cases of patients with non-neovascular retinal pigment epithelium (RPE) protrusion. All patients also had hyperreflective material (HRM)—a catch-all term for areas of greater signal intensity—in the neurosensory retina. Outcome measures of patient characteristics, changes in SD-OCT findings and symptom fluctuations were determined through clinical examination, color fundus photography, fluorescein angiography, SD-OCT and OCT angiography.
The study researchers found that all cases displayed RPE protrusion and HRM with dilated choroidal veins—both hallmarks of pachychoroid disease. Conversely, none were found to have macular neovascularization. The HRM spontaneously improved in 81.8% (n=9) of cases without any intervention. However, it did result in RPE alterations called pachychoroid pigment epitheliopathy (PPE) or focal choroidal excavation. These cases saw improved symptoms of metamorphopsia and distortion without treatment. The remaining 18.2%, or two cases, still saw persistent HRM during follow-up.
The study authors noted that there are some cases of non-neovascular pachychoroid disorder with hyperreflective signal, “which might be a new entity of pachychoroid spectrum disease or an early stage of PPE or choroidal excavation. These cases should not be misdiagnosed as macular neovascularization, and careful observation is necessary.”
In previous studies, hyperreflective findings at the subretinal space were reported as a biomarker for worse visual acuity in AMD patients and is also known to have components of neovascular tissue, fibrosis, hemorrhage and exudation likely comprised of serum, fibrin and inflammatory cells. This study found no neovascular tissue, fibrosis or hemorrhage consistent with HRM, suggesting it was a kind of exudation.
Hyperreflectivity was seen in the outer plexiform and nuclear layers, as well as the subretinal space. Prior studies explain that hyperreflective foci are seen in many chorioretinal diseases, defined as hyperreflective speckling in the neurosensory retina. Four cases in this study displayed these foci with acoustic hyperreflectivity behind the HRM. The foci have been thought to originate from displaced RPE cells, activated microglia cells and lipid extravasation.
With regard to the cases that improved spontaneously, most displayed pachychoroid pigment epitheliopathy or focal choroidal excavation. Since both are usually asymptomatic, the authors believe the HRM caused these symptoms. Abnormalities that produce hyperreflective signal may activate the RPE apical surfaces, phagocytosed by RPE cells, and then result in morphologic features similar to PPE. Some eyes showed focal choroidal excavation, the cause of which remains uncertain; however, some reports describe it as being linked to congenital choroidal abnormalities, while others associate its presence with inflammatory diseases such as multiple white dot syndrome, multifocal choroiditis or Vogt-Koyanagi-Harada disease.
The researchers explained that differential diagnoses in such presentation were neovascular diseases of AMD and idiopathic choroidal neovascularization. These were ruled out since no cases presented with macular neovascularization. Despite this, they concluded in their paper that “it is important to check the existence of macular neovascularization by multimodal imaging and differentiate non-neovascular lesions with HRM” from either similar entity.
Maruyama-Inoue M, Yanagi Y, Mohamed S, et al. Hyperreflective material in patients with non-neovascular pachychoroid disease. BMC Ophthalmol. June 6, 2023. [Epub ahead of print]. |


