 |
|
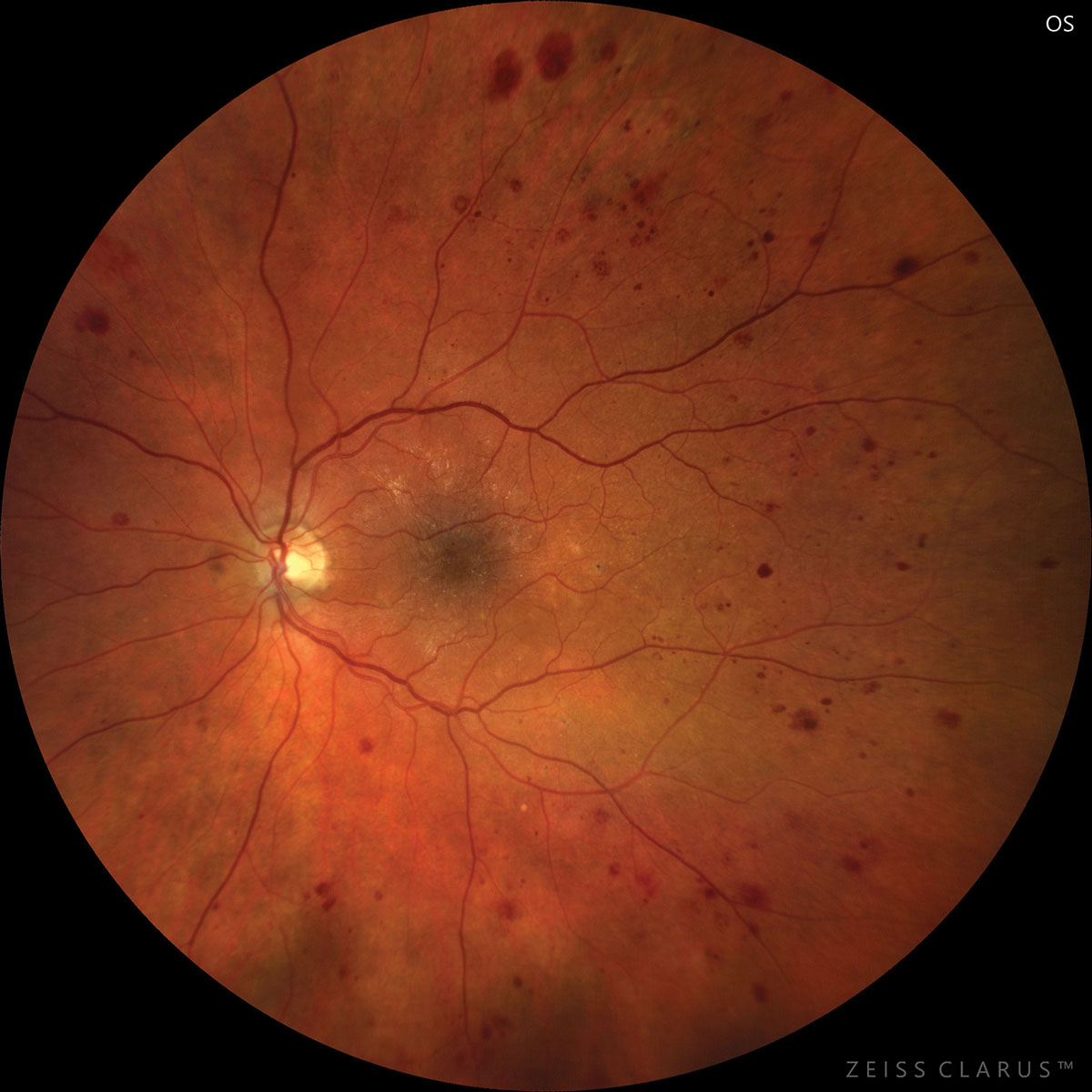
Patients with DME may have more microaneurysms detectable on OCT-A. Photo: Josh Z. Yuen, OD, PhD. Click image to enlarge. |
Many potential factors have already been identified to predict response to anti-VEGF agents, including pre-treatment central retinal thickness, HbA1c level, presence of subretinal fluid, intraretinal cysts and renal disease. Despite these being known, there remains the problem that a significant proportion, around 25%, of those with the condition either do not respond or show insufficient response to repeated anti-VEGF injections. Since the cost of these agents can be a major burden for patients, one study takes aim to identify a potential new biomarker as a predictor of therapeutic response.
The research focused on analyzing microaneurysms (MAs), since they are a bellwether of development and progression of DME, but its relationship to anti-VEGF treatment response remains unclear. Subsequently, the researchers sought to clarify the relationship between MA distribution and patient response to anti-VEGF treatment.
Differences in distribution of MAs between groups were investigated and the number of MAs were measured using fluorescein angiography (FA), indocyanine green angiography (ICGA) and OCT angiography (OCT-A).
Interestingly, more MAs were seen in the nasal area of the non-responder group than the responder group in pre-treatment IA. Pre-treatment FA and OCT-A, on the other hand, displayed no significant difference between the groups. Based on these findings, MAs in the nasal macula detected by pre-treatment ICGA may indicate anti-VEGF therapy resistance.
More specifically, the researchers point out that the presence of a large microaneurysm through ICGA detection of the nasal macula is indicative of physiologically and anatomically severe DME, and they aptly suggest that such severe cases are likely to resist anti-VEGF therapy.
As for why ICGA was the only technique that displayed significant differences, the researchers have their thoughts on that, too. OCT-A may have masked the detection of MAs because of noise, resulting in lower detection sensitivities in this study compared to other reports. ICGA, however, is a useful technique for identifying cases of DME that exhibit leaking spots or larger capillaries. Because of its ability to identify larger areas, ICGA may help characteristically visualize microaneurysms because it has a low detection sensitivity.
A previous report mentions that the size of MAs correlates with improvement of DME after anti-VEGF treatment, and the researchers of this study identify that smaller MAs may respond better to therapy than larger ones. This is due to their finding that the responder group had many small MAs of detectable size for FA but not for ICGA, while microaneurysms detected on the nasal macula using ICGA were less than both FA and OCT-A in the responder group. As a result, once microaneurysms become large enough to be detectable by indocyanine green angiography (but not FA or OCT-A), they may affect the treatment’s efficacy.
The authors extend that their findings can be applicable to practitioners, as they “recommend that clinicians confirm the presence of MAs in the nasal macula, as shown by ICGA, as a predictor of therapeutic response to anti-VEGF therapy in patients with treatment naïve DME.”
Hatano M, Higashijima F, Yoshimoto T, et al. Evaluation of microaneurysms as predictors of therapeutic response to anti-VEGF therapy in patients with DME. PLoS One. November 28, 2022. [Epub ahead of print]. |


