 |
|
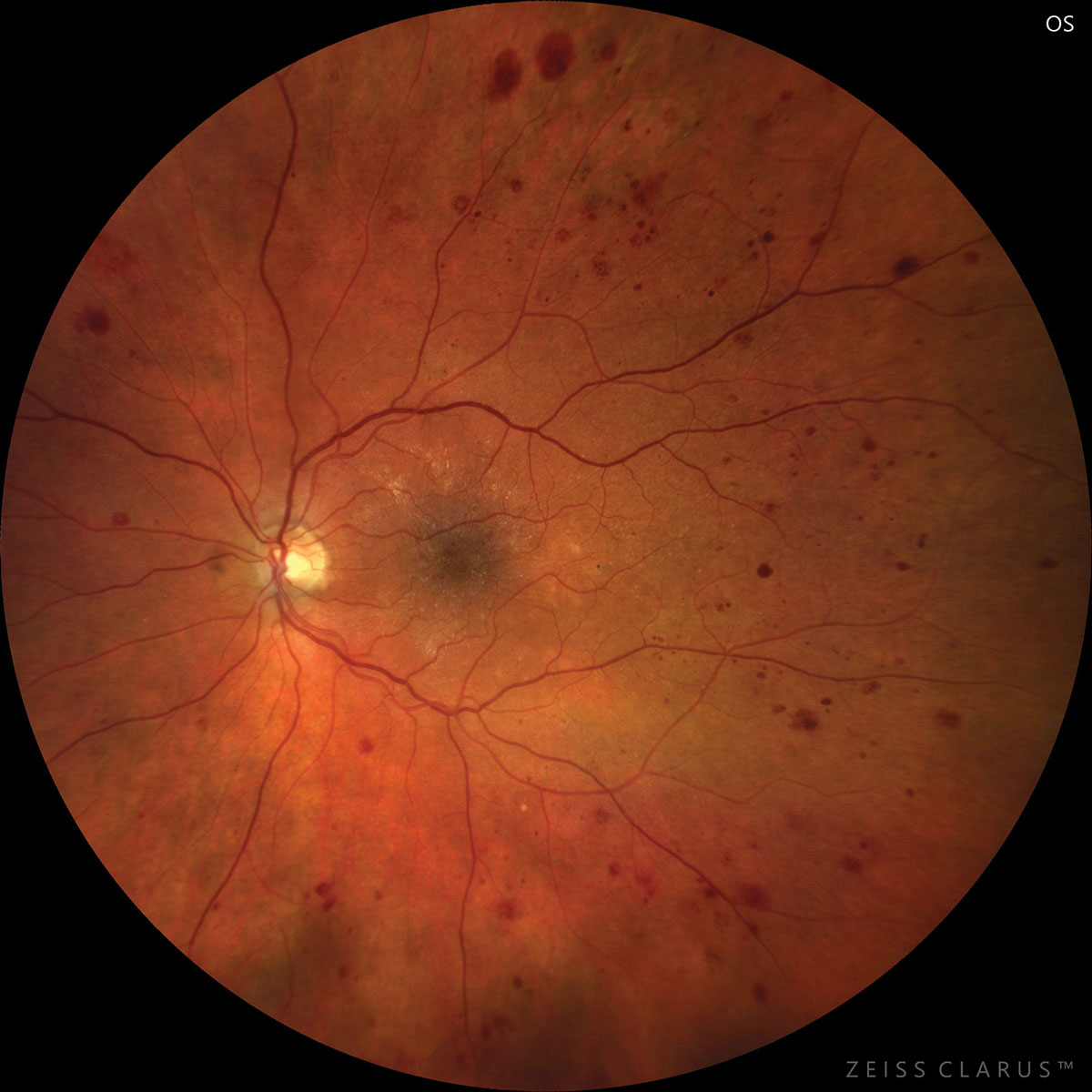
DR lesion distribution differs among Caucasians, Latinos, South Asians and East Asians, this study observed. Photo: Jay Haynie, OD. Click image to enlarge. |
While diabetic retinopathy (DR) lesions can present either peripherally or centrally, the variation among prevalence between the two types is not as well documented. One new study sought to outline whether there is a notable distribution of such DR lesions across multiple ethnicities.
The retrospective study included 226 total eyes with retinopathy. Of those, 51 were East Asian, 102 were South Asian, 30 were Caucasian and 43 were Latino. All eyes were evaluated with ultra-widefield images, with manual annotations made about DR lesion classification (peripheral or central). The distribution percentages for each were then compared among different ethnicities.
Main findings included East Asian eyes demonstrating a much higher peripheral lesion distribution (86.3%), while South Asian eyes exhibited the opposite, with a centralized lesion distribution of 64.7%. Even in consideration of the treatment-naïve subset of eyes, the results were the same. Compared with treatment naïve eyes with nonproliferative DR, the percent distribution of peripheral lesions in East Asian eyes varied significantly from other ethnicities. Of the East Asian group, 65.8% of eyes with peripheral findings displayed lesions across multiple ETDRS fields, while in the South Asian group, 55.6% displayed only one affected field.
To highlight the importance of this discovery, the authors mention another study that, using UWF imaging, found DR lesions may lie outside the seven ETDRS fields even in early disease. Specifically, eyes with peripheral distribution had a baseline 3.2-fold increased risk of two-step or more DR progression and a 4.7-fold increased progression risk to proliferative retinopathy after four years. Hence, identifying peripheral retinal lesions, especially in ethnicities that may show increased percentages, becomes important for the clinician.
Despite the pathophysiology of peripheral findings remaining unclear, multiple possibilities have been mentioned. One study reports differential diameter dilation in macular and peripheral arterioles may play a role in the uneven distribution. Another postulates that increased retinal nonperfusion is at work peripherally. These biological factors become less clear when considering ethnic variation, though.
The researchers additionally point out the possibility of genetic factors at play, such as a phenotypic variation. They report that genetic difference has already explained ethnic variation in early age-related macular degeneration lesions, and it is reasonable to consider this phenomenon to have a similar explanation, at least in part.
Authors do note that patients in this study were recruited from different geographic locations, so other factors may be contributing to this result, such as access to healthcare, socioeconomic status and metabolic control.
For clinicians, the authors say that the peripheral distribution’s connection to a higher risk of progression is a potentially important finding, making it a concern to be on the lookout for this type of manifestation. They conclude that “future longitudinal studies will be required, however, to determine whether this higher risk also translates to East Asian patients.”
He Y, Verma A, Nittala M, et al. Ethnic variation in diabetic retinopathy lesion distribution on ultra-widefield imaging. Am J Ophthalmol. 2022. [Epub ahead of print]. |


