OCT has come to dominate the assessment of glaucomatous damage by precisely measuring the thickness of the retinal nerve fiber layer (RNFL). However, much of its clinical value depends on the accuracy of the reference database (RDB)—formerly called “normative database”—used for comparison. These datasets have been criticized in recent years for underrepresenting various patient groups and thus over- or understating the likelihood of glaucoma. Manufacturers are working to improve RDB accuracy in a number of ways.
Current RDBs primarily consider patient age and disc area, potentially leading to false positives or missed diagnoses. To address this limitation, a recent study investigated the relationship between anatomical parameters of healthy eyes and OCT measures of circumpapillary RNFL (cpRNFL) thickness, aiming to identify additional factors that could enhance diagnostic accuracy. The lead author of the study was Donald Hood, MD, he of the widely used “Hood Report” for glaucoma assessment and an expert on the disease. Topcon supported the research and its Maestro OCT was used in the study, but the results and their implications are not limited to the company’s products.
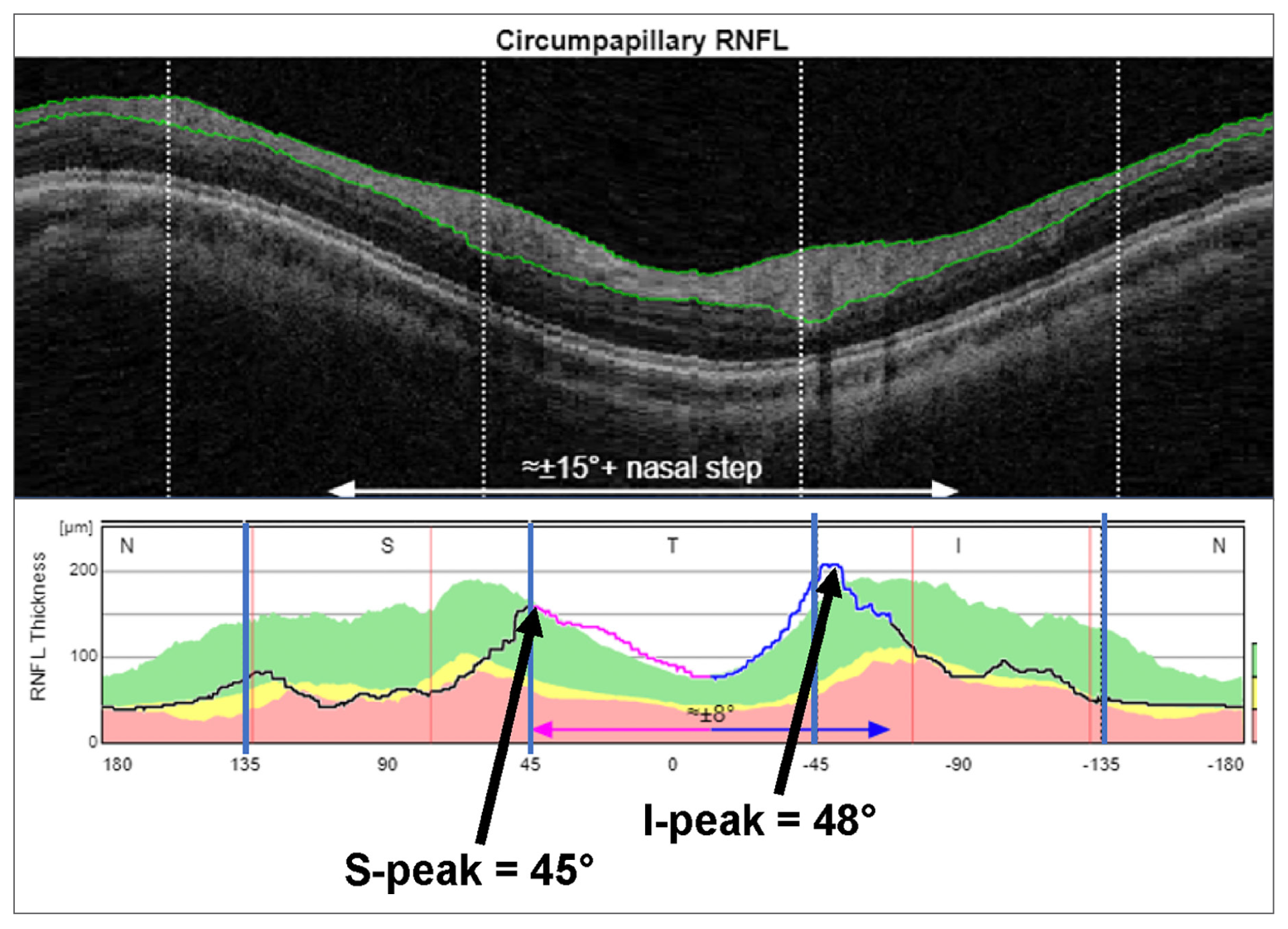 |
| This image from the study shows the location of the superior and inferior peaks of the cpRNFL thickness curve, two of the four parameters associated with abnormal RNFL values in healthy eyes. Photo: Hood DC, Transl Vis Sci Technol. 2024;13(4):27. Click image to enlarge. |
OCT scans of 396 healthy eyes in a commercial reference database were analyzed. The study focused on four anatomical parameters: fovea-to-disc distance, location of the superior peak of the cpRNFL thickness curve (S-Peak), location of the inferior peak of the cpRNFL thickness curve (I-Peak) and estimated axial length.
The findings revealed that these anatomical parameters exhibited stronger correlations with cpRNFL thickness in specific quadrants compared to age or disc area. All four parameters listed above were significantly associated with abnormal cpRNFL values. The study authors suggest that using an RDB that incorporates these parameters into OCT measures can improve the diagnostic accuracy of glaucoma assessments, identify false positives and enhance clinical decision-making.
“Currently, only age and disc area are included in estimating percentiles of the cpRNFL quadrant and global cpRNFL thickness of the Maestro reference database,” the authors wrote in their article for Translational Vision Science & Technology. They asserted, “The fovea-to-disc distance, S-Peak location, I-Peak location and perhaps mirror position as a proxy for axial length should be considered as additional factors. We predict that including these parameters will improve diagnostic accuracy in real-world clinical settings.” The authors note, however, that “this predicted improvement in accuracy requires testing with a reference database sampled from a real-world database.”
Overall, this study underscores the potential of incorporating anatomical parameters into OCT reference databases to enhance the detection and understanding of glaucomatous damage.
Hood DC, La Bruna S, Durbin M, et al. Anatomical features can affect OCT measures used for clinical decisions and clinical trial endpoints. Transl Vis Sci Technol. 2024;13(4):27. |


