 |
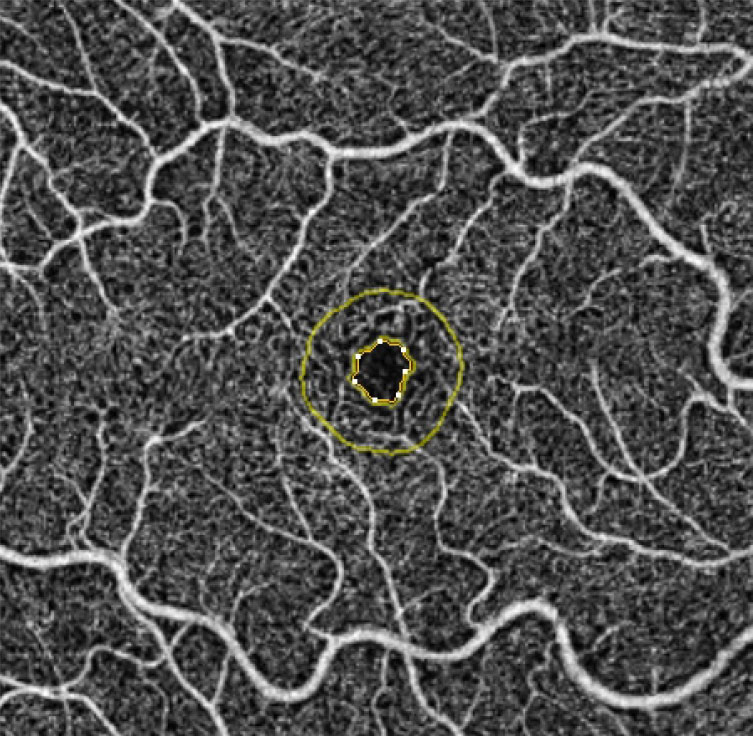
| OCT-A may have utility as a biomarker for Parkinson’s disease, as these patients have retinal microvascular alterations appearing to be most distinct in the foveal region. Photo: Julie Rodman, OD. Click image to enlarge. |
Over time, and especially without treatment, Parkinson’s disease can lead to numerous impairments, including cognitive impairment, autonomic dysfunction, sleep disturbances and visual symptoms. A definitive diagnosis is currently only possible through histopathological examination, highlighting the need for an effective, noninvasive diagnostic test to enable earlier detection and treatment of the progressive disorder. To explore the potential application of OCT-A as a biomarker for Parkinson’s, researchers recently performed a systematic review and meta-analysis on current evidence in the literature and found that certain metrics were different between patients with and without the disease.
Thirteen observational studies from various online databases were included in the review and analysis. A total of 925 eyes made up the Parkinson’s disease group, while 1,501 eyes were controls.
The meta-analysis found that, compared with healthy controls, the foveal region of Parkinson’s disease patients had a significantly lower vessel density in the superficial capillary plexus. However, no significant differences were observed between patients vs. controls in the foveal avascular zone, superficial capillary plexus, parafoveal and perifoveal regions or deep capillary plexus.
In their paper published in Eye, the researchers explained that these results show that “the fovea is more sensitive to vessel density changes in Parkinson’s disease, specifically in the superficial capillary plexus.” They added that this finding is “in line with other studies that discovered significantly lower measurements of superficial capillary plexus vessel density in the fovea of Parkinson’s disease patients.” One such study “showed that the alternations in the retinal microvasculature appear more specifically in the foveal region.” The study also observed that microvascular parameters such as perfusion and skeleton density, lacunarity of capillaries and fractal dimension were greater in Parkinson’s patients.
In contrast, the research team pointed out, another study from the meta-analysis didn’t observe any significant changes in the foveal superficial capillary plexus, but it did find “an association between intraretinal layer thickness and superficial capillary plexus vessel density, which was present only in the foveal region in Parkinson’s disease patients who were at an early stage.” The researchers suggested that some of these discrepancies could be attributable to the differences in OCT-A algorithms used in the various studies.
The researchers concluded that while the current analysis suggests OCT-A metrics could potentially act as a biomarker for earlier and more accurate Parkinson’s diagnosis, longitudinal studies are still needed to assess the dynamics of retinal vascular changes over time as the disease progresses. Additionally, they pointed out in their paper that “the OCT-A algorithms and interchangeability between OCT-A devices require further standardization to draw clinical conclusions regarding their utility.”
Salehi MA, Rezagholi F, Mohammadi S, et al. Optical coherence tomography angiography measurements in Parkinson’s disease: a systematic review and meta-analysis. Eye. February 14, 2023. [Epub ahead of print]. |


