 |
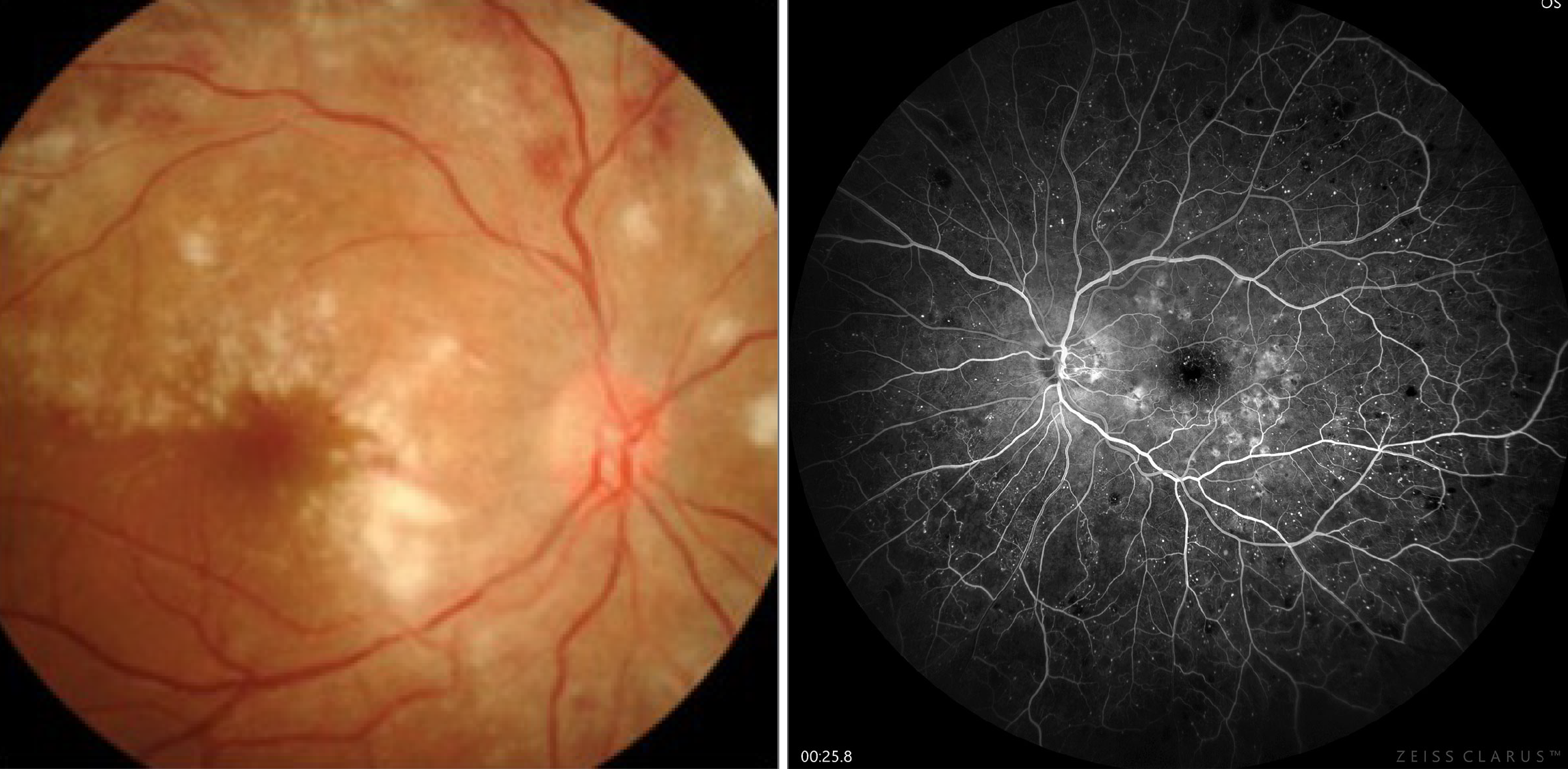
Intermediate uveitis has been linked to an earlier onset of posterior vitreous detachment, which prevents the further progression of DR into proliferative stages. Photo: Michael Trottini, OD, and Candice Tolud, OD; Jay Haynie, OD. Click image to enlarge. |
Despite the well-documented pathophysiological mechanisms, there have been very few studies describing the clinical characteristics of eyes with co-existing diabetic retinopathy (DR) and uveitis. Vasculitis-induced ischemia in uveitis is known to exacerbate pre-existing hypoxia in DR and worsen that disease. Researchers in India have recently described the clinical profile and complications of diabetic retinopathy and uveitis in eyes with concurrent conditions, as well as to evaluate associations based on the site of primary inflammation, DR grade and complications of each. They found that the development of uveitis in eyes with preexisting diabetic retinopathy is associated with significant morbidity and visual consequences.
Electronic medical records of 66 patients with co-existing diabetic retinopathy and uveitis were evaluated in this study, which was published recnetly in Ophthalmology Science. Of the 132 eyes, all had DR and 97 eyes had uveitis (35 unilateral and 31 bilateral cases). Mean age of patients was 53.4 years, duration of diabetes was 10.5 years and duration of uveitis was 61.3 months.
In this patient cohort, 54.6% of uveitis patients had anterior uveitis, 20.6% had intermediate uveitis, 10.3% posterior uveitis and 14.4% panuveitis. The researchers noted that 49.5% eyes had proliferative DR (PDR) changes. There was a higher proportion of PDR cases among anterior (56.6%) and posterior (70%) uveitis as well as panuveitis (64.3%), with the difference in anterior uveitis cases approaching statistical significance. Conversely, significant intermediate uveitis cases had nonproliferative changes (80%). “Poor glycemic control, a known risk factor for uveitis in diabetic patients, also influences DR status,” the researchers wrote in their paper.
Final BCVA was significantly poorer in the group with uveitis. The proportion of fibrovascular proliferations, tractional detachments and iris neovascularization among proliferative retinopathy eyes with uveitis (14.6%, 18.8% and 12.5%, respectively) was higher than those without uveitis (5.3%, 10.5% and 5.3%). Among uveitis cases, 58.5% eyes developed cataracts, 44.3% had posterior synechiae, 12.3% developed secondary glaucoma, 4.1% had epiretinal membrane, 4.1% had band-shaped keratopathy and 1.0% developed macular neovascularization.
“Treatment should aim at limiting the duration and intensity of inflammation,” the authors suggested. “Strict glycemic control is essential for reducing inflammation and preventing the progression of DR to more advanced proliferative stages.”
Mohapatra A, Sudharshan S, Majumder PD, et al. Clinical profile and ocular morbidities in patients with both diabetic retinopathy and uveitis. Ophthalmol Sci. March 7, 2024. [Epub ahead of print]. |


