 |
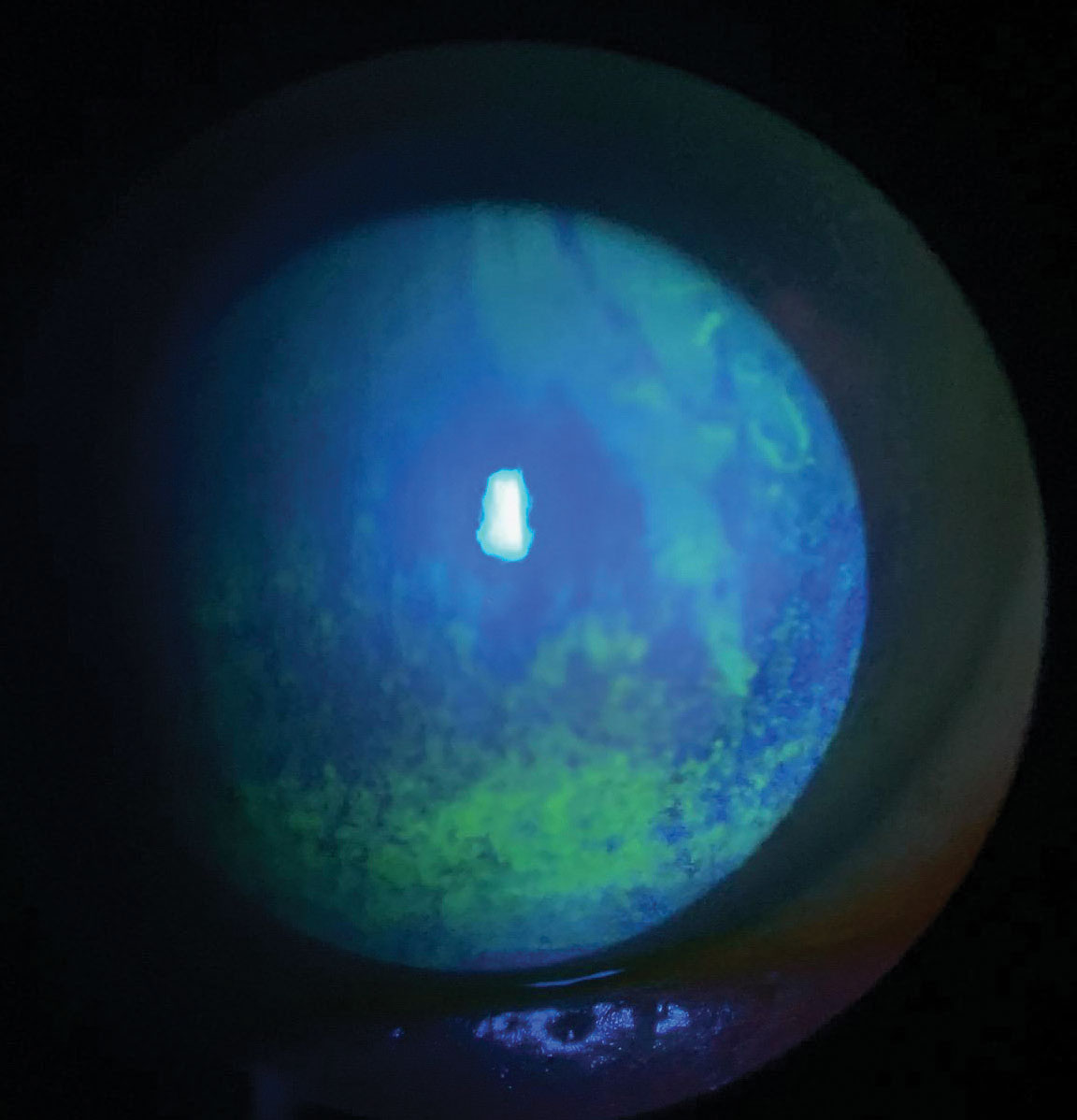
| In this study, patients with DED who wore contacts showed increased ocular surface staining. Photo: Scott G. Hauswirth, OD. Click image to enlarge. |
Several studies have found conflicting results on the combination of dry eye disease (DED) and contact lens wear and whether corneal sensitivity and corneal nerve density have an effect on these patients. In a recent study, researchers investigated ocular surface alterations and in vivo confocal microscopic characteristics of the cornea in DED with contact lens wear.
Sixty participants were divided into three groups: DED with contact lens wear, DED without contact lens wear and controls. Basal tears and in vivo confocal microscopy images of the cornea were collected, and nerve morphology and dendritic cell density in corneal subbasal nerve images were calculated. Multiplex bead analysis was used to assess interleukin (IL)-6, IL-1b, tumor necrosis factor, nerve growth factor and substance P in tears.
Patients with DED with contact lens wear showed increased ocular surface staining which may contribute to various contact lens-related factors. Also found was greater epithelial damage, elevated inflammatory cytokines and neuromediators in tears and higher corneal dendritic cell density than patients with DED without lens use.
Although the DED with contact lens wear group showed higher substance P levels than the other two groups, the differences were not significant, which was consistent with a previous study. The authors hypothesized that there could be two contributory mechanisms.
“On the one hand, substance P can be released directly from sensory nerve terminals in response to stimulation and is implicated in corneal cold nociception and pain transmission,” they explained. “Wearing contact lenses significantly increased evaporation of the tear film and decreased ocular surface temperature dramatically, stimulating nerve terminals to release substance P. High levels of substance P in tears may facilitate nociceptive sensitization of the ocular surface. The positive correlation between substance P levels and ocular surface disease index scores in the DED with contact lens wear group may support this hypothesis.”
On the other hand, they explained, some immune cells have been discovered to release substance P, implying that substance P plays a significant part in the immune response. “Contact lenses are presented to the ocular surface as a foreign body, triggering the innate immune system, which may contribute to the higher substance P levels in tears of patients with DED with contact lens wear,” the study authors noted.
When patients in the two study groups were compared with healthy controls, morphological alterations in the corneal nerve were discovered. Additionally, there was a negative correlation between corneal nerve fiber density and years of contact lens wear, as well as a positive correlation between corneal dendritic cell density and years of contact lens wear. These findings suggested that, while corneal nerve density and dendritic cell density fluctuated during the initial stage of contact lens wear, long-term contact lens wear results in dendritic cell activation and corneal nerve damage.
Yang T, Ma B, Xie J, et al. Evaluation of ocular surface characteristics in dry eye disease with and without soft contact lens wear: a comparative study. Eye Contact Lens. May 17, 2022. [Epub ahead of print]. |


