 |
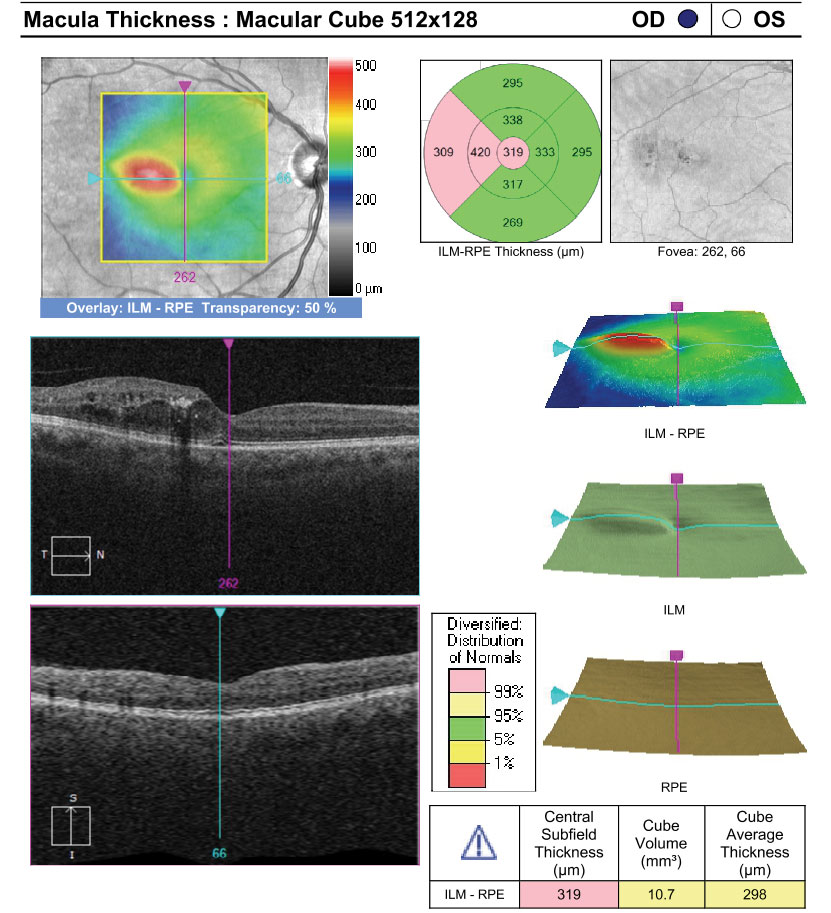
An increase in retinal extracellular fluid could signal an increased possibility of vision loss in patients with CI-DME. Photo: Anna Bedwell, OD, and Larissa Krenk, OD. Click image to enlarge. |
It is important to characterize progression of macular edema in the initial stages of diabetic retinopathy (DR) in order to identify opportunities for early intervention before disease progression and vision loss occur. Subclinical center-involved diabetic macular edema (CI-DME) has been proposed as a predictor for the development of CI-DME, and many believe it would be beneficial to use OCT as an objective measurement of CI-DME and a reference to identify DME needing close surveillance to guarantee timely treatment.
Researchers in Portugal sought to characterize the prevalence and three-year progression of CI-DME in minimal to moderate nonproliferative (NP) DR using OCT and measurements of retinal fluid. Subclinical CI-DME did not appear to be a predictor for development of CI-DME. However, the team noted a progressive increase in retinal extracellular fluid registered in the eyes with subclinical CI-DME and CI-DME with vision loss, which suggests a relevant role for retinal extracellular fluid accumulation and chronicity in vision loss development in the initial stages of macular edema.
The study consisted of 74 eyes from 74 patients who were followed in a three-year prospective, longitudinal, observational cohort of patients with type 2 diabetes and and NPDR (ETDRS grades 10 to 47) using SD-OCT, OCT-A and OCT-Leakage, an algorithm capable of performing automated analyses of the abnormal retinal extracellular space by identifying and measuring sites of lower optical reflectivity. The team studied participants’ eyes four times in one-year intervals and categorized them as minimal, mild and moderate NPDR using seven-field ETDRS grading. Retinal edema was measured by central retinal thickness (CRT) and retinal fluid by using optical reflectivity ratios obtained with the OCT-Leakage algorithm. Vessel density was measured by OCT-A. Thinning of the ganglion cell and inner plexiform layers (GCL + IPL) was examined to identify retinal neurodegenerative changes.
CI-DME was identified in the first visit in 9% of eyes in ETDRS groups 10 to 20, 10% of eyes in ETDRS group 35 and 15% of eyes in ETDRS groups 43 to 47. “The results reported here confirm that eyes in the initial stages of diabetic retinopathy in type 2 diabetes individuals show evidence of CI-DME identified by OCT in a relatively small number of eyes and that CI-DME shows similar prevalence in eyes with different grades of ETDRS severity below level 47,” the study authors wrote. “In summary, CI-DME, i.e., ≥2 standard deviation CRT increase, can occur very early in the disease process and is, in general, not apparently related to DR severity.”
The eyes with CI-DME and subclinical CI-DME showed a progressive increase in retinal extracellular fluid during the three-year period of follow-up. The eyes with CI-DME and increased retinal extracellular fluid accumulation were associated with vision loss. Changes in CRT and low optical reflectivity ratios did not appear to be directly associated with changes in vessel density (ischemia) or GCL + IPL thinning (neurodegeneration).
The researchers believe that identification and quantification of abnormal extracellular fluid accumulation in the diabetic retina and its location in the different layers of the retina may explain progression of macular edema and associated vision loss.
“Abnormal accumulation of retinal extracellular fluid appears to be a good indicator for the need for close monitoring with potential for early treatment,” they concluded.
Lobo C, Santos T, Marques IP, et al. Characterisation of progression of macular oedema in the initial stages of diabetic retinopathy: a three-year longitudinal study. Eye (Lond). January 22, 2022. [Epub ahead of print]. |


