One of the major visual disabilities for patients with advanced AMD involving geographic atrophy (GA) is the gradual decline and then permanent loss of reading ability within the central field. Although photoreceptors are lost within areas of GA, the inner retinal neurons largely survive. A prosthetic device called Prima (Pixium Vision) is a wireless subretinal receiver in which photovoltaic pixels directly convert projected light into patterns of electric current to reintroduce visual information a by electrical stimulation of second-order neurons—the bipolar cells.
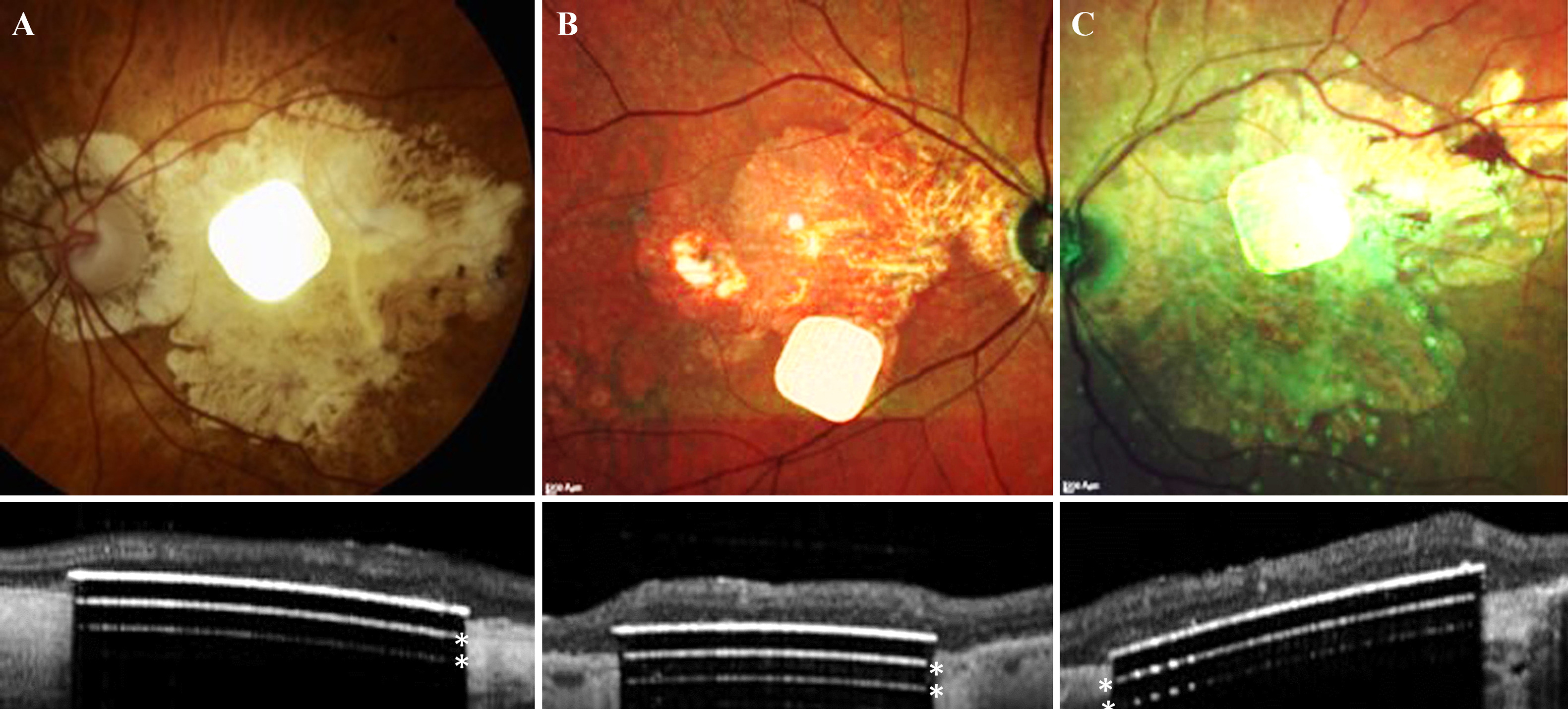 |
| Subretinal implantation of Prima in subjects with GA suffering from profound vision loss due to AMD is feasible and well tolerated, according to this study. These photos and OCT scans show placement in the three successful subjects. (The two white lines below the implant surface (*) are OCT artifacts due to strong light reflection from the implant surface.) Photo: Meqit MMK, et al. Ophthalmol Sci. March 7, 2024. Click image to enlarge. |
While Prima is not yet available, a recent study published in Ophthalmology Science assessed its efficacy and safety for improving visual acuity (VA) in five patients with GA due to AMD. Up to four years after implantation, the subretinal microchip (activated by a pair of light-sensing glasses) enabled subjects to read at least four additional lines on the vision chart compared with their natural vision. “Prosthetic central vision provided by photovoltaic neurostimulation enabled patients to reliably recognize letters and sequences of letters, and with zoom it improved VA of up to eight ETDRS lines,” the authors wrote in their paper.
The current version of this implant is a 2mm wide (corresponding to about 7° of the visual angle in a human eye) and 30μm thick chip, containing 378 pixels of 100μm in width. Images captured by the camera using augmented reality (AR) glasses are processed and projected onto the implant using near-infrared (880nm) light. Photovoltaic pixels convert this light into electric current flowing through the retina between the active and return electrodes, which stimulates the nearby inner retinal neurons. Their responses then pass through the retinal neural network to ganglion cells, harnessing the residual retinal signal processing.
In one patient the implant was incorrectly inserted into the choroid. Another died 18-months post-implantation due to unrelated reasons. ETDRS VA results for the remaining three subjects were reported.
Without zoom, VA closely matched the pixel size of the implant: 1.17 pixels, corresponding to mean logMAR 1.39, or Snellen 20/500, ranging from 20/438 to 20/565. Using zoom at 48 months, subjects improved their VA by 32 ETDRS letters vs. baseline. Natural peripheral visual function in the treated eye did not decline after surgery, nor during the 48 months follow-up period.
“The subretinal photovoltaic array provided form vision with letter acuity closely matching the 100μm pixel size in patients with geographic atrophy, with no decline in eccentric natural acuity over a four-year period,” the researchers wrote. “The transparent AR glasses allow simultaneous use of the prosthetic central and natural peripheral vision. Using electronic zoom, patients demonstrated clinically meaningful and statistically significant improvements in vision.”
Most of the device- and procedure-related non-serious adverse events occurred within the first six months post-implantation, and none led to any long-term safety issues. These include the microcysts discovered in three subjects (two occurred nine months post-implantation) and the asymptomatic choroidal neovascular membrane in one subject (which occurred 31 months after implantation).
“Unlike the current pharmacological treatments for geographic atrophy, which aim to slow down the growth of atrophic lesions without any functional improvement in VA, our results demonstrate restoration of central vision in the former scotoma,” the researchers noted. “Reduced pixel size in the future implants may further improve the prosthetic VA to much higher levels.”
Meqit MMK, Le Mar Y, Olmos de Koo L, et al. Prosthetic visual acuity with the PRIMA subretinal microchip in patients with atrophic age-related macular degeneration at four years follow-up. Ophthalmol Sci. March 7, 2024. [Epub ahead of print]. |


