 |
|
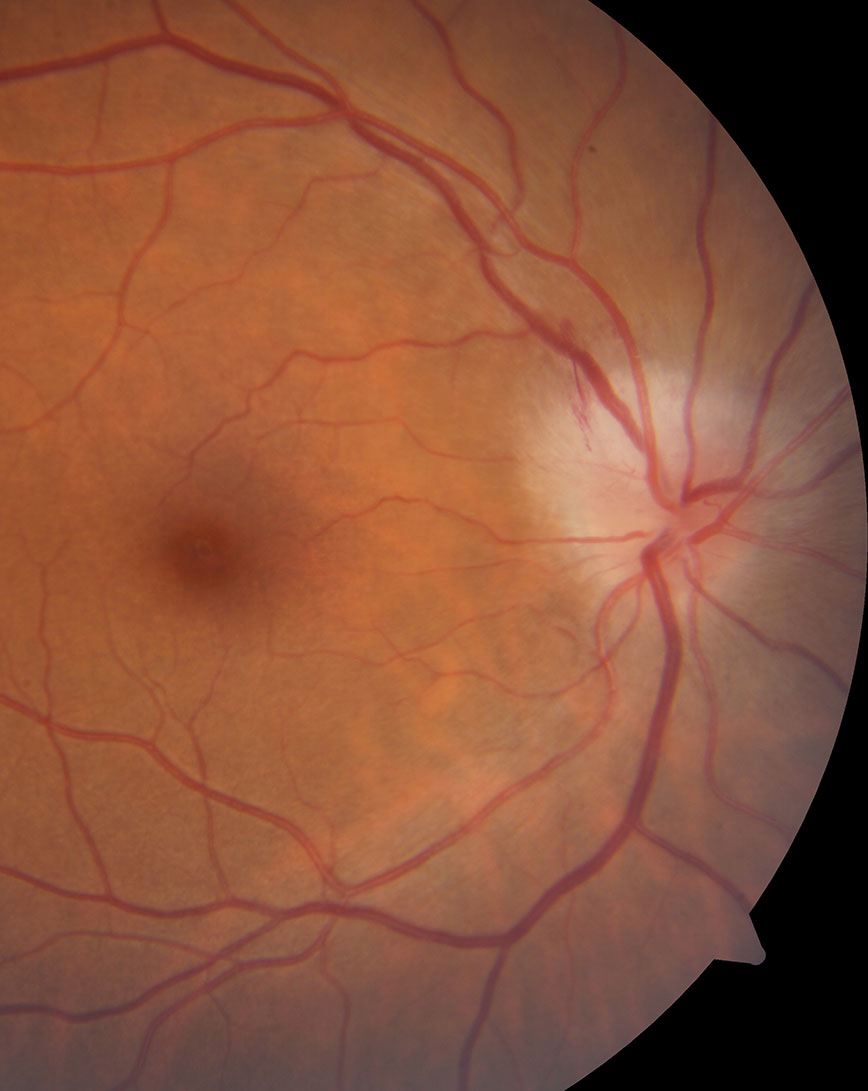
Only 12% of optic neuritis patients who underwent plasma exchange ended with a visual acuity of worse than 20/40. Photo: Nate Lighthizer, OD. Click image to enlarge. |
A team of researchers wanted to elucidate just how effective the therapeutic option of plasma exchange (PLEX) may be for optic nerve inflammation from varying causes. The study was retrospective and internationally spanned many centers, evaluating optic neuritis (ON) outcomes after PLEX treatment. The outcomes were then compared to data from the Optic Neuritis Treatment Trial (ONTT).
“The exact mechanism of PLEX is unclear, but it is thought to provide benefit by rapid removal of plasma antibodies, immune complexes and cytokines that are involved in demyelinating disease and inflammation,” the researchers wrote in their paper for American Journal of Ophthalmology.
Evaluated was a total of 317 patients who experienced 395 ON attacks. Median age was observed at 37 years old and 71% of all participants were female. ON was caused by many different conditions. The two most to common were multiple sclerosis and myelin oligodendrocyte glycoprotein antibody–associated disease (MOGAD), followed by several other demyelinating diseases of the central nervous system, arising from idiopathic and other reasons.
The average time from vision loss onset to receiving PLEX was 2.6 weeks, with average visual acuity at time of PLEX was count fingers, with median final visual acuity to be 20/25. The only etiology with a significantly different outcome was MOGAD, which displayed better outcomes than the others.
A total of 20.5% of ON attacks resulted in a visual acuity of 20/200 or worse. These poor outcomes were associated with older age, worse visual acuity at time of PLEX and longer delay receiving the treatment. A final visual acuity below 20/40 occurred in only 12% of PLEX-treated patients, which was lower than the ONTT rate of 33% treated with intravenous methylprednisone instead. Overall, most ON attacks improved following PLEX, with better outcomes observed in attacks of similar severity in the ONTT.
The researchers of the study note that finding worse vision at onset understandably results in worse recovery, even with the treatment of PLEX. A similar intuitive sense applies to older patients, who also displayed worse outcomes. The median age of those with poorer outcomes was over a decade higher than those with better outcomes. The researchers postulate this could be caused by a reduction in ability to repair and remyelinate as one ages.
Eyes with previous optic neuritis displayed worse outcomes than those without after PLEX treatment. Researchers of the study point to two reasons for this. First, damage from older optic neuritis attacks could result in the optic nerve having less reserve to recover after another, later attack. The other possibility is of prior attacks with residual visual loss incapable of improving past an impaired baseline following another recurring attack.
Taking all their findings into consideration, the authors of the study believe their results “warrant further exploration and provide the backbone for a future prospective randomized clinical trial of PLEX treatment for optic neuritis,” they noted in their paper.
Chen JJ, Flanagan EP, Pittock SJ, et al. Visual outcomes following plasma exchange for optic neuritis: An international multicenter retrospective analysis of 395 optic neuritis attacks. Am J Ophthalmol. 2023. [Epub ahead of print]. |


