 |
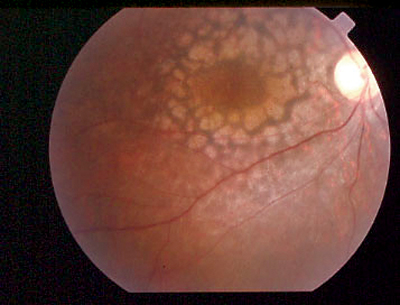
| Leber’s congenital amaurosis (pictured) and related RPE65 conditions were generally responsive to gene therapy, particularly in the pediatric population of participants. Photo: Sherry Bass, OD. Click image to enlarge. |
Inherited retinal degeneration (IRD) resulting from associated biallelic mutations of the RPE65 gene typically ends in blindness by the third or fourth decade of life. The mutation can manifest in a spectrum of retinal phenotypes, including Leber’s congenital amaurosis, early-onset severe retinal dystrophy and juvenile retinitis pigmentosa. Three years ago, the FDA approval of subretinal voretigene neparvovec (Luxturna, Spark Therapeutics) received worldwide acclaim as the first commercialized gene therapy to counteract progress of RPE65-IRD.
New research appearing in Ophthalmology covers the impact that voretigene neparvovec treatment has on outcomes in a series of patients treated since approval. Patients with RPE65-IRD were treated by one surgeon at a single center with the injection and oral immunosuppression as was recommended by manufacturer recommendation. A total of 30 eyes from 19 patients was analyzed—including 10 pediatric patients less than 20 years of age—and ages spanning from eight to 40 years old.
After comparing data from baseline to 24 months post-treatment, the study researchers found the fovea was completely or partially detached in 16 eyes, attached in 12 and not assessable in two upon intraoperative imaging. Median best-corrected visual acuity (BCVA) was better in the pediatric group at baseline and did not change significantly. Meaningful BCVA loss occurred in four out of 18 adult eyes, while meaningful gain was observed in two out of 18 adult eyes and two out of eight pediatric ones. Low-luminance visual acuity and scotopic two-color threshold perimetry improved in pediatric cases, while scotopic blue full-field stimulus threshold testing improved in all ages, but especially with children. New chorioretinal atrophy was observed in 13 out of 26 (50%) eyes at the site of the bleb and/or peripheral of vascular arcades. Mean retinal thickness also remained relatively stable, with an average thickness of 166.7µm at baseline and 157.7µm at month 12.
The authors elaborate on their findings, making sure to point out that significant loss of BCVA did not correlate with developing new or accentuated chorioretinal atrophy, an observation that aligns with other research. Median sum of total degrees at baseline was four times greater in the pediatric group than in adults, displaying the progressive nature of underlying degenerative processes. Five pediatric patients saw considerable improvement of up to 50% (190 sum degrees) at month 12, which corresponds to a gain of five years’ Goldmann visual fields. Consequently, this treatment effect would be relevant for better patient mobility and would favor younger patient treatment.
However, the authors do report “severe vision loss in individual patients that appear to be treatment related in patients whom we treated only unilaterally.” With some hands-on experience, the team now suggests “to prolong the treatment interval of the second eye to at least three months, since half of the unilaterally treated patients were unhappy because of loss of BCVA that did not appear predictable from the baseline data.”
Lorenz B, Künzel SH, Preising MN, et al. Real-world experience with Voretigene Neparvovec gene augmentation therapy in RPE65-mutation associated inherited retinal degeneration. Ophthalmology. September 11, 2023. [Epub ahead of print]. |


