 |
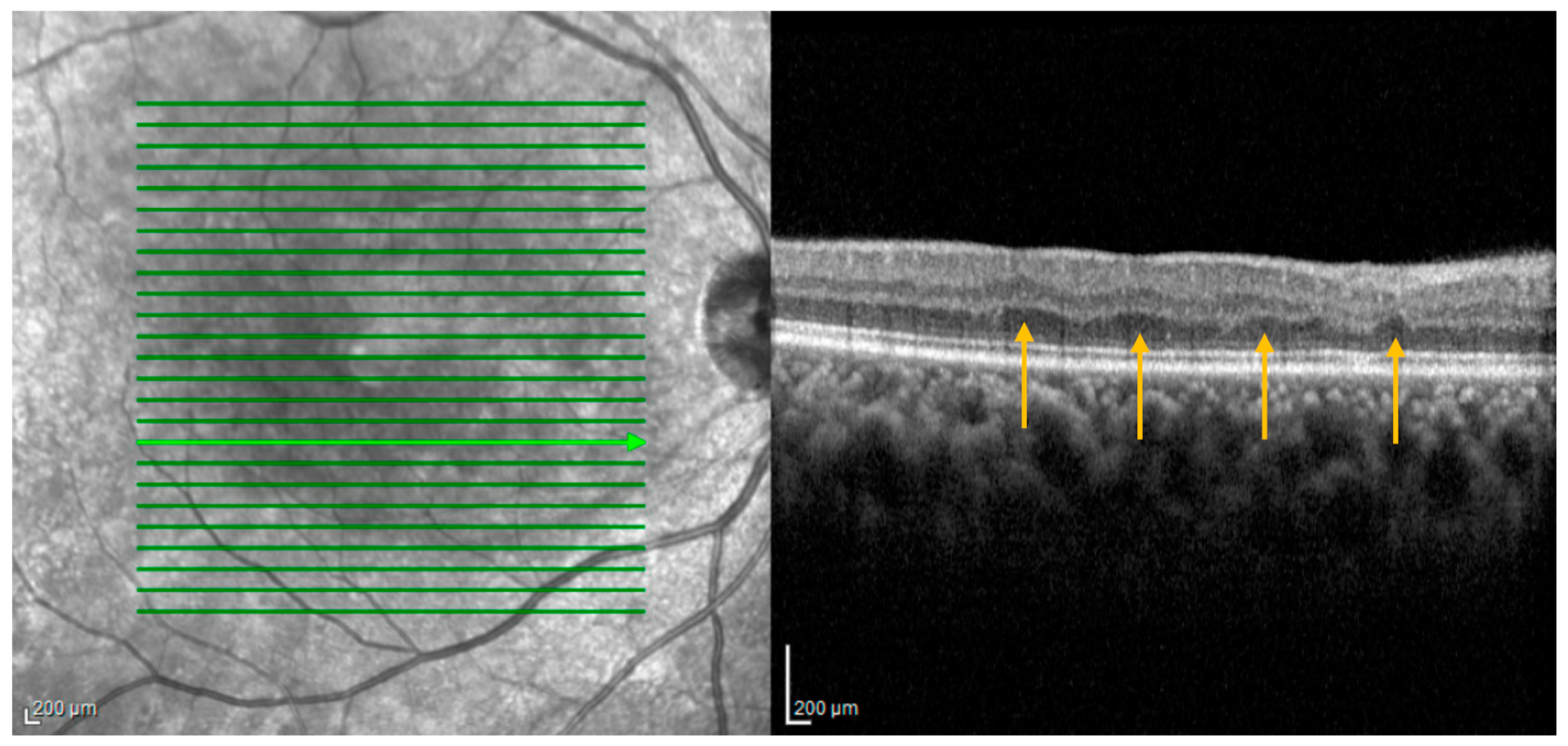
| RIPLs are thought to arise at the sites of previous middle retinal layer infarcts, potentially evolving as a subsequent manifestation of paracentral middle maculopathy, wherein the hyperreflective inner nuclear band observed during the acute phase gradually undergoes atrophy over time. Photo: Colcombe J, et al. J. Pers. Med. 2023, 13:1564. Click image to enlarge. |
A recently described anatomical finding called retinal ischemic perivascular lesions (RIPLs), detected via OCT, is indicative of certain systemic cardiovascular conditions, including diabetes both with and without diabetic retinopathy and hypertension. More recently, they have been linked with cardiovascular conditions of coronary artery disease, atrial fibrillation and carotid artery stenosis. RIPLs are characterized by focal atrophy of the inner nuclear layer accompanied by secondary expansion of the outer nuclear layer, resulting in an undulating appearance of the middle retinal layers.
Since recent reports highlight that RIPLs can be useful in identifying subclinical cardiovascular disease, one new study wanted to determine if RIPLs are a marker of myocardial infarction (MI) in a cohort of patients with coronary artery disease (CAD). Researchers did indeed find such an association.
The retrospective investigation included 317 consecutive CAD patients who underwent spectral domain OCT (SD-OCT). Of all patients, 17% had a history of MI. A markedly higher prevalence of RIPLs was seen in the MI group at 59.3% compared with the non-MI group of 35.7%. After analysis, the researchers determined that presence of RIPLs was significantly associated with MI even after adjusting for age, sex, smoking status, hypertension, diabetes, dyslipidemia and BMI.
In their paper for American Journal of Ophthalmology, the authors note that their findings are consistent with one previous study also reporting an observed higher (but not statistically significant) count of RIPLs in MI patients vs. those without. The present study confirmed these preliminary results in a larger patient base.
Another prior investigation reported RIPLs were found in 90% of patients with mild hypertension and only in 17% of healthy participants. Similarly, RIPLs have been observed in diabetic patients with and without diabetic retinopathy, with one previous report showing 94.9% of patients with diabetic retinopathy and 53.8% without exhibiting them on OCT. However, this current study found equal hypertension and diabetes prevalence among patients with and without MI, suggesting these risk factors aren’t contributing to increased RIPL prevalence in the Mi group.
The authors also elaborate on the association of smoking status with MI in their analysis. Only discordant results are currently available pertaining to cigarette smoking on retinal capillary plexus density. Despite this, one study has identified smoking as an independent risk factor for reduced retinal deep capillary plexus perfusion on OCT angiography.
Finally, the authors suspect that the pathophysiology of RIPLs in the setting of MI may be attributed to retinal hypoperfusion of the deep capillary plexus, either from microemboli formation or reduced ventricular ejection fraction.
Looking toward future use of their results, the authors posit that, “should this association be confirmed by prospective studies, this would suggest that SD-OCT screening for RIPLs in CAD patients could be an important stratification tool for those at risk of developing MI.”
They add that “these findings emphasize the critical role of RIPL detection in patients with coronary artery disease and support a growing consensus for cardiovascular evaluation in patients with isolated RIPL.”
Bousquet E, Santina A, Au A, et al. Retinal ischemic perivascular lesions are associated with myocardial infarction in patients with coronary artery disease. Am J Ophthalmol. March 27, 2024. [Epub ahead of print]. |


