 |
|
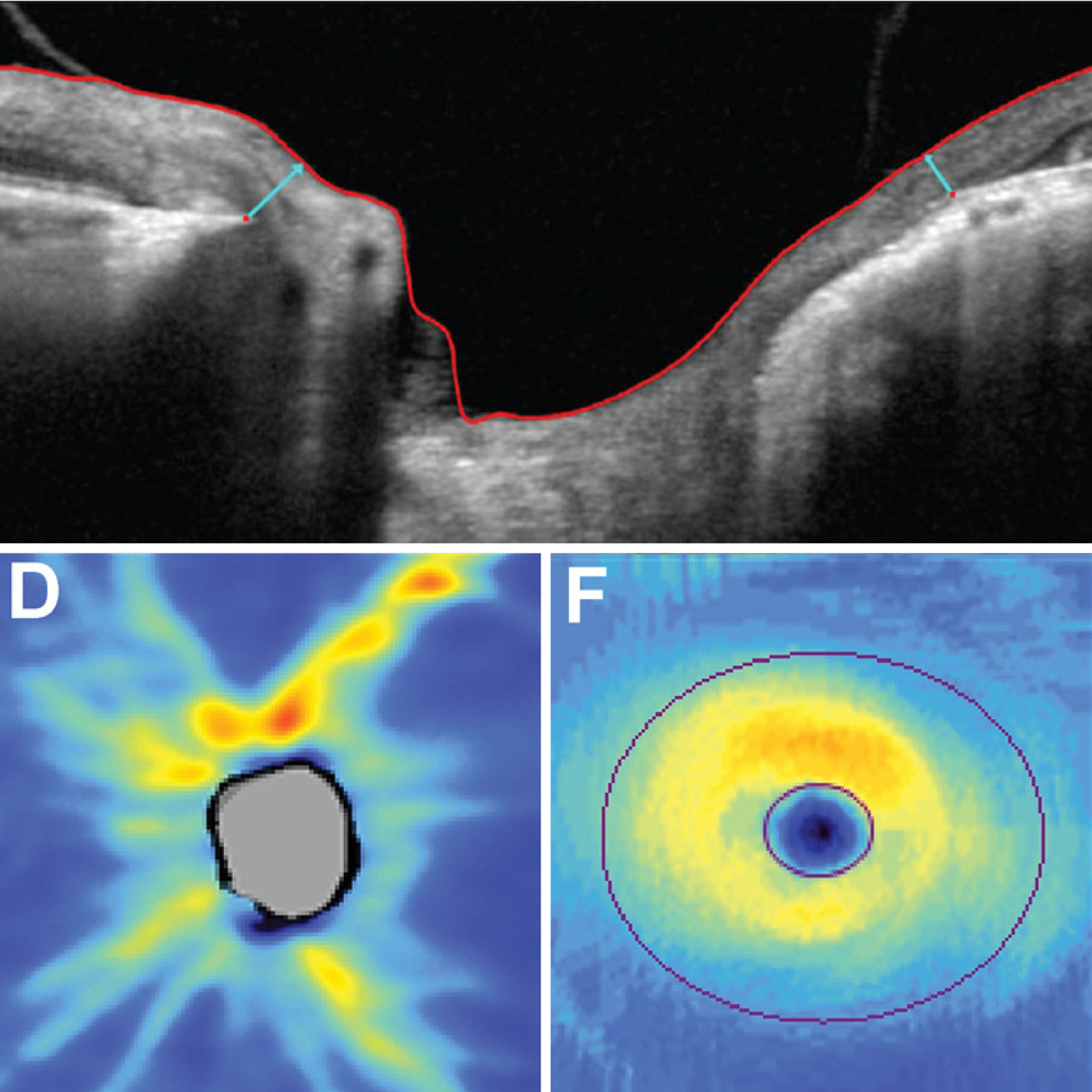
RNFLT may be more useful than MRW in early glaucoma assessment because of its previously reported lower variability and reduced sensitivity to intraocular pressure changes. Photo: Chris Wroten, OD, and James Fanelli, OD. Click image to enlarge. |
Optometrists and ophthalmologists routinely track changes in retinal nerve fiber layer (RNFL) thickness—and, more recently, minimum rim width (MRW) of Bruch’s membrane opening—in glaucoma patients and suspects. These two metrics seem to correspond in some ways. In a new study, researchers took a deep dive into this subject and aimed to determine whether OCT-derived rates of change in MRW are associated with and can potentially predict corresponding alterations in RNFLT in people with glaucoma.
The primary analysis used a series of up to five visits over approximately a two-year period. The authors did not find evidence of a clinically significant time lag for either MRW nor RNFL changes. “This suggests that even though change might be detected sooner using one measure than the other, there is no predictable causative link whereby change in MRW consistently precedes similar changes in RNFL thickness or vice versa,” the researchers explained in their paper for Translational Vision Science & Technology.
These findings appear to contrast previous studies suggesting that MRW changes manifest prior to RNFL thinning in glaucoma, and there are several reasons why. First, glaucoma is more common in older patients and previous data suggests that tissues found in the optic nerve hypoplasia region such as the sclera and lamina cribrosa stiffen significantly as a function of age. “Consequently, there is less susceptibility to mechanical deformation at the ONH. This may result in MRW thinning concurrently to RNFLT as seen in this study or that the structural damage for the two parameters has a similar onset,” the authors wrote.
Also, transient changes in cupping of the ONH occur as a result of fluctuating IOP levels and cannot be feasibly controlled for in human experimental studies. “Therefore any IOP measures or parameters impacted by IOP changes such as MRW, are a mere snapshot of these fluctuating changes and may not reflect the more chronic structural glaucomatous changes in the eye,” they noted.
Third, the authors explained that it cannot be ruled out that the hypothesized six-month time lag between MRW and RNFL changes may be the wrong time interval. “A time lag of much less than six months remains consistent with our results but would be of less translational interest because glaucoma suspects are typically only seen in clinics once or at most twice per year, so such a time lag would be too short to be relevant clinically.”
Lastly, it remains possible that MRW does indeed change earlier than RNFLT as glaucoma develops, as suggested by previous literature. “In this scenario, the first stage would consist of both conformational and remodeling-based changes at the ONH that alter MRW but not RNFLT; followed by a second stage at which axon loss occurs and both MRW and RNFL thickness change concurrently,” the authors explained. “Our results then suggest that the transition between those stages occurs relatively abruptly, rather than a gradual transition over several years, which would be detectable as a time lag in our models.”
As RNFL thickness is less variable to assess (due to being less impacted by IOP fluctuations), the authors suggest that this parameter is of more use in the early assessment of glaucomatous progression.
Higgins BE, Yang H, Gardiner SK. The temporal relation between rates of retinal nerve fiber layer and minimum rim width changes in glaucoma. Trans Vis Sci Technol. April 5, 2024. [Epub ahead of print.] |


